Issues in the management of esophageal cancer and geriatric patients
Introduction
Cancer is a disease associated with aging and we need to be prepared for this demographic shift as our average cancer patient is getting older. In the United States and United Kingdom, the median age of patients with esophagogastric cancer is 68–70 years old and greater than 30% of patients are over the age of 75 at the time of diagnosis (1,2). Similarly in China, the majority of patients are age 60 years and older, with the highest incidence rates of cancer occurring in patients aged 75–85 years old (3).
Despite the increased incidence of cancer in the elderly, older patients are less likely to be referred to a cancer specialist, and even if referred, less likely to receive treatment, irrespective of tumor stage or comorbidities (4). Surgical resection or combined modality treatments with radiation and chemotherapy are often felt to be too toxic for most elderly patients with localized esophageal cancer despite the recent trials showing decreases in recurrence and improvements in overall survival. While there are clearly physiologic changes that occur with aging and patient-related factors such as comorbidities, functional status, and limited social support can affect the ability to deliver and tolerate cancer treatment, chronological age alone should not dictate a patient’s treatment management. This review will describe issues specific to older patients, the utilization of geriatric assessment (GA) tools, and how to apply geriatric principles to patients with esophagogastric cancers.
Overview of physiologic versus chronological age
In clinical practice, it becomes very clear that not all 75-year-old patients are alike. In determining appropriate therapy and management for an older patient, it is essential to determine a patient’s physiological age, rather than chronological age. Geriatricians often use the term, “frailty”, versus fit older adults to distinguish between patients of the same chronological age who may be vastly different in terms of functioning, independence, and performance status. Frailty is a geriatric syndrome that is distinct and independent from medical comorbidities (5). Markers of frailty include sarcopenia, low physical activity and endurance, and walking performance. It is thought to involve decreased physiologic reserve, chronic inflammation, and immune dysregulation leading to loss of capability to withstand stressors and resulting vulnerabilities (6). Frailty has been predictive for increased falls, worsening disability, hospitalization, and increased mortality (7).
In the cancer population, a frail older patient is one who will be at higher risk of treatment toxicity and complications (8). Studies have shown that frailty is associated with increased postoperative complications in elderly cancer patients undergoing colorectal and gynecological surgery (9,10). Evaluation and identification of frail older patients is important for several reasons. Recognizing frailty can lead to distinguishing patients who are at higher risk of adverse outcomes versus fit older individuals. This may provide information to guide treatment planning and decision-making in older cancer patients.
GA tools
There are several tools that have been developed to identify frail older adults, including the frailty phenotype (11) and the frailty index, a 70-item tool (12). Although these frailty tools can be helpful especially in the research setting to define frailty, a GA provides a more comprehensive understanding of a patient’s physiological age and to help determine fit vs. frail (13). Comprehensive GA is used to detect vulnerabilities in older patients and to devise treatment strategies. In oncology practice, it has been used as a tool to help risk-stratify patients prior to planned therapy. The International Society of Geriatric Oncology developed a consensus statement on GAs in older cancer patients (14). A GA is comprised of validated measures that assess age-related problems not typically identified in a routine history and physical examination. The domains include functional status, mobility, nutritional status, social support, cognition, and polypharmacy (Table 1). Components of the GA have been shown to be predictive of treatment related toxicity in chemotherapy patients, postoperative complications, as well as overall survival (13-17).
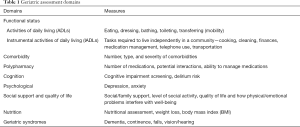
Full table
In the oncology setting, a full GA may not be feasible due to constraints on time or resources. Tools based on the GA have been developed for use to determine a patient’s chemotherapy risk. Examples of tools include the Cancer-Specific GA (CSGA) developed by Hurria and the Cancer and Aging Research Group and the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score (18,19). The CSGA tool was prospectively studied in 500 patients aged ≥65 years with cancer receiving chemotherapy. All patients underwent a full GA. A predictive model was developed comprised of 11 risk factors including GA variables along with patient demographic and clinical variables to predict grade 3 to 5 toxicity with chemotherapy administration. Higher scores were associated with higher rates of toxicity. In this study, physician rated Karnofsky Performance Status Score (KPS) did not identify older adults at increased risk for chemotherapy toxicity. The CSGA is brief, can be largely self-administered, and can be completed by the majority of older patients without assistance. While such tools are not a replacement for a full GA, it can be a helpful screening tool in identifying higher risk patients who may benefit from a more comprehensive GA prior to initiation of therapy. The National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology now includes the “Older Adult Oncology” section which provides excellent detail and further reading on this subject (20). Unfortunately given the limited data, there are no disease specific recommendations for esophagogastric cancers.
Application to esophageal cancer patients
How do we best apply these data and guidelines to older patients with esophageal cancer? For older patients with localized disease, surgery remains the mainstay of treatment. Esophagectomy is a high-risk surgery with serious potential postoperative complications. There are retrospective surgical series looking at the risks of esophagectomy in older patients, and while the rates of increased risks are debated, most of the data suggests that older patients are at increased risk for cardiovascular and pulmonary complications (21-24). A large SEER-Medicare database review of esophagectomy outcomes showed that operative mortality increases with age, up to 13.4% in patients 70–79 years old, and 19.9% in patients over the age of 80 (25). Given the potentially high morbidity and mortality rate as well as the high risk of recurrence when patients have lymph node positive disease, the role of esophagectomy needs to be carefully considered in an older patient (26,27). These patients should undergo preoperative GA and follow-up in the postoperative period with close monitoring for geriatric syndrome such as delirium and polypharmacy and have a plan in place for rehabilitation. For other patients who are medically not optimal surgical candidates or who declined surgery, definitive chemoradiotherapy may achieve long-term disease control and is a potentially curative option, especially for patients with squamous cell cancers.
In all patients with esophageal cancer, and particularly for those who are undergoing potentially aggressive and curative treatment, an issue of concern is nutritional status, a key component of the GA. Malnutrition has been associated with reduced response to treatment and survival in esophageal cancer patients, as well as detrimentally affecting quality of life and increasing health care costs. In older patients, poor nutritional status has been found to be a predictor of early death
For older patients with advanced or metastatic esophagogastric cancer, improving on maintaining quality of life and symptom relief are as important as prolonging survival. Best supportive care with symptom management is the appropriate option for patients who have compromised functional status and for those individuals who decline chemotherapy. Palliative chemotherapy should be individualized based on the patient’s performance status and comorbidities. The CSGA tool, while it has not been validated in this specific disease population, may be helpful to stratify older patients to more aggressive chemotherapy regimens (combination chemotherapy) vs. single agent chemotherapy regimens. Combination chemotherapy can result in higher response rates and may be appropriate for robust older patients. The FLOT65+ study showed that in very robust patients age 65 years or older doublet and triplet chemotherapy was feasible to administer. The triplet combination (infusional 5-fluoruracil, leucovorin, oxaliplatin with docetaxel) improved response rates and progression free survival in patients aged between 65 and 70 years old, albeit with significant increased toxicity compared to the doublet chemotherapy. However, in patients aged 70 years and older or those with metastatic disease, there was no benefit for the triplet combination. As such, three drug combination chemotherapy should not be used in almost all older patients given the very high rates of grade 3–4 toxicities (33).
In older patients undergoing chemotherapy, the most common complications include myelosuppression, gastrointestinal toxicity, renal toxicity, and neurotoxicity. Chemotherapy can also affect cognition, function, and mood (34). Combination of these issues can result in increased risk of delirium, falls, and loss of independence. With age, renal glomerular filtration rate (GFR) decreases which can result in delayed elimination of many drugs, including oxaliplatin, cisplatin, and capecitabine. Dose adjustment to the GFR should be considered for these drugs to decrease systemic toxicity and careful review of home medications needs to be undertaken given polypharmacy in older patients with multiple comorbidities. With platinum agents and taxanes, neurotoxicity results in high falls risks for older patients and requires close monitoring.
The field of oncology is changing rapidly with new drug innovations and increased molecular understanding of the biology of cancer. The demographics of our cancer population are changing just as rapidly, with the higher age-specific incidence of cancer. Oncologists need more knowledge and information about how to best treat our older patients. This will require understanding the physiological changes in the older patient and how to properly select patients for effective and safe cancer treatment. With the application of geriatric principles and assessment in cancer patients, we are in the beginning stages of increasing our knowledge base. Clearly there is more work to be done. Ongoing and future studies are applying this information to stratify older patients to treatment groups based on risk factor and to devise practical interventions to better support patients through cancer therapy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- Howlader N, Noone AM, Krapcho M, et al. editors. SEER Cancer Statistics Review, 1975-2009 (Vintage 2009 Populations), National Cancer Institute. Bethesda, MD, based on November 2011 SEER data submission, posted to the SEER web site, April 2012. Available online: http://seer.cancer.gov/csr/1975_2009_pops09/
- Chen W, Zheng R, Zeng H, et al. Annual report on the status of cancer in China, 2011. Chin J Cancer Res 2015;27:2-12. [Crossref] [PubMed]
- Steyerberg EW, Neville B, Weeks JC, et al. Referral patterns, treatment choices, and outcomes in locoregional esophageal cancer: A population-based analysis of elderly patients. J Clin Oncol 2007;25:2389-96. [Crossref] [PubMed]
- Fedarko NS. The biology of aging and frailty. Clin Geriatr Med 2011;27:27-37. [Crossref] [PubMed]
- Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging 2014;9:433-41. [PubMed]
- Shamliyan T, Talley KM, Ramakrishnan RA. Association of frailty with survival: A systematic literature review. Ageing Res Rev 2013;12:719-36. [Crossref] [PubMed]
- Baijal P, Periyakoil V. Understanding frailty in cancer patients. Cancer J 2014;20:358-66. [Crossref] [PubMed]
- Courtney-Brooks M, Tellawi AR, Scalici J, et al. Frailty: an outcome predictor for elderly gynecologic oncology patients. Gynecol Oncol 2012;126:20-4. [Crossref] [PubMed]
- Tan KY, Kawamura YJ, Tokomitsu A, et al. Assessment for frailty is useful for predicting morbidity in elderly patients undergoing colorectal cancer resection whose comorbidities are already optimized. Am J Surg 2012;204:139-43. [Crossref] [PubMed]
- Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146-56. [Crossref] [PubMed]
- Rockwood K, Song X, Macknight C, et al. A global clinical measure of fitness and frailty in elderly People. CMAJ 2005;173:489-95. [Crossref] [PubMed]
- Korc-Grodzicki B, Holmes HM, Shahrokni A. Geriatric assessment for oncologist. Cancer Biol Med 2015;12:261-74. [PubMed]
- Wildiers H, Heeren P, Puts M, et al. International society of geriatric oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol 2014;32:2595-603. [Crossref] [PubMed]
- Audisio RA, Bozzetti F, Gernnari R, et al. The surgical management of elderly cancer patients: recommendations of the SIOG surgical task force. Eur J Cancer 2004;40:926-38. [Crossref] [PubMed]
- Caillet P, Canoui-Poitrine F, Vouriot J, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J Clin Oncol 2011;29:3636-42. [Crossref] [PubMed]
- Soubeyran P, Fonck M, Blanc-Bisson C, et al. Predictors of early death risk in older patients treated with first-line chemotherapy for cancer. J Clin Oncol 2012;30:1829-34. [Crossref] [PubMed]
- Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol 2011;29:3457-65. [Crossref] [PubMed]
- Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 2012;118:3377-86. [Crossref] [PubMed]
- National Comprehensive Cancer Network. Older Adult Oncology (Version 2.2017). Available online: http://www.nccn.org/professionals/physician_gls/pdf/senior.pdf
- Swisher SG, DeFord L, Merriman KW, et al. Effect of operative volume on morbidity, mortality, and hospital use after esophagectomy for cancer. J Thorac Cardiovasc Surg 2000;119:1126-32. [Crossref] [PubMed]
- Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med 2002;346:1128-37. [Crossref] [PubMed]
- Bailey SH, Bull DA, Harpole DH, et al. Outcomes after esophagectomy: a ten-year prospective cohort. Ann Thorac Surg 2003;75:217-22. [Crossref] [PubMed]
- Ra J, Paulson EC, Kucharczuk J, et al. Postoperative morality after esophagectomy for cancer: development of a preoperative risk prediction model. Ann Surg Oncol 2008;15:1577-84. [Crossref] [PubMed]
- Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer. J Am Coll Surg 2007;205:729-34. [Crossref] [PubMed]
- Abate E, DeMeester SR, Zehetner J, et al. Recurrence after Esophagectomy for Adenocarcinoma: Defining Optimal Follow-Up Intervals and Testing. J Am Coll Surg 2010;210:428-35. [Crossref] [PubMed]
- Gu Y, Swisher SG, Ajani JA, et al. The number of lymph nodes with metastasis predicts survival in patients with esophageal and esophagogastric junction adenocarcinoma who receive preoperative chemoradiotherapy. Cancer 2006;106:1017-25. [Crossref] [PubMed]
- Conti S, West JP, Fitzpatrick HF. Mortality and morbidity after esophago-gastrectomy for cancer of the esophagus and cardia. Am Surg 1977;43:92-6. [PubMed]
- Clavier JB, Antoni D, Atlani D, et al. Baseline nutritional status is prognostic factor after definitive radiochemotherapy for esophageal cancer. Dis Esophagus 2014;27:560-7. [Crossref] [PubMed]
- Di Fiore F, Lecleire S, Pop D, et al. Baseline nutritional status is predictive of response to treatment and survival in patients treated by definitive chemoradiotherapy for a locally advanced esophageal cancer. Am J Gastroenterol 2007;102:2557-63. [Crossref] [PubMed]
- Baldwin C, McGough C, Norman AR, et al. Failure of dietetic referral in patients with gastrointestinal cancer and weight loss. Eur J Cancer 2006;42:2504-9. [Crossref] [PubMed]
- Won E, Ilson DH. A Nutritional Management Algorithm in Older Patients With Locally Advanced Esophageal Cancer. ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US), 2000. Cited 2017 Jul 21. NLM Identifier: NCT02027948. Available online: http://clinicaltrials.gov/show/NCT02027948
- Al-Batran SE, Pauligk C, Homann N, et al. The feasibility of triple-drug chemotherapy combination in older adult patients with oesophagogastric cancer: a randomized trial of the Arbeitsgemeinschaft Internistische Onkologie (FLOT65+). Eur J Cancer 2013;49:835-42. [Crossref] [PubMed]
- Naeim A, Reuben D. Geriatric syndromes and assessment in older cancer patients. Oncology (Williston Park) 2001;15:1567-77. [PubMed]


