The prospective of laparoscopic pancreaticoduodenectomy for cancer management
Introduction
Laparoscopic pancreaticoduodenectomy (LPD) remains one of the most advanced laparoscopic procedures. Owing to the evolution in laparoscopic technology and instrumentation within the past decade, LPD is beginning to gain wider acceptance. While minimally invasive approaches are more feasible and very safe, some pancreatic surgeries are still performed in an open procedure because of the location and intimate relationship of the pancreas to major blood vessels, the reconstruction complexity of a pancreatoduodenectomy and the technical difficulty in performing such a minimally invasive approach (1). Modern medicine has introduced laparoscopic surgery that has revolutionized the field of pancreatic surgery so that, by now, surgical procedures for either benign or malignant pancreatic disease can be performed laparoscopically. The general differences between an open approach and a laparoscopic surgery are the methods of access and exposure and the degree of operative trauma (2). In line with significant development and maturation of surgical technologies, the numbers of such laparoscopic pancreatic surgeries have increased each year. However, although clinical procedures were initiated around 2 decades ago, laparoscopic pancreatic surgery, specifically LPD, is still in its infancy; thus, certain innovations and novel strategies to manage this kind of procedure still need to be explored.
Methods and materials
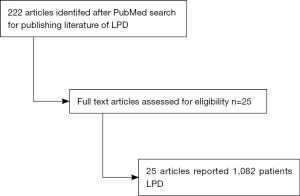
A literature search was conducted in PubMed. Papers in laparoscopic distal pancreatectomy and robotic pancreatic procedure were not included in the review. The final search was completed on December, 2016 and revealed 222 articles and papers written in English containing more than 25 publications of LPD were selected. The total number of patients analyzed was 1,082 patients, and the largest series. Six of these studies come from the United States, 1 from France, 5 from South Korea, and 1 from India, 2 from Japan, 5 from China, 1 from Italy, 1 from Germany, 2 from UK. In the literature review, both descriptive and comparative studies were found. We extracted technical, perioperative and intraoperative data. This included conversion rate, operative time, and intraoperative blood loss. We also collected information on hospital length of stay, pancreatic leak, mortality. Oncologic data including number of lymph nodes removed, and resection was also recorded (Figure 1).
Results
LPD
The first LPD procedure was described by Gagner and Pomp in 1994 (3). Despite being first carried out 2 decades ago, it has not yet gained universal acceptance and popularity as it requires highly advanced technical skills with a lengthy learning curve, requiring a longer operative time (4). Despite the difficulty and complexity of this surgical procedure, LPD has been progressively developed in specialized centers due to the availability of newer technologies, successful application of laparoscopy in other complex abdominal surgeries and the motivation by surgeons to embrace innovation in the modern world (5). Recent reports on a large series of LPD demonstrated that the procedure might not only be feasible, but that it might have advantages as compared with open pancreaticoduodenectomy (OPD). According to Li et al. (6), their experience of LPD showed shortened hospitalization time and that operation time for experienced surgeons was significantly shorter than their previous attempts. Accordingly, blood loss was less, overall length of hospital was shorter, post operation pain was less and a faster recovery time were just some of the perceived benefits of LPD over open procedures (7).
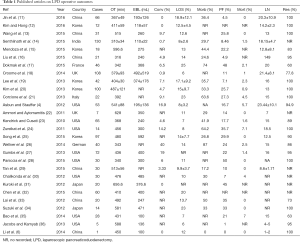
Boggi et al. (5) has published a large review incorporating 25 articles wherein four techniques currently used for LPD (pure, hand-assisted, robot-assisted laparoscopy and laparoscopic-assisted surgery) were summarized. There were a total of 746 LPD surgeries between 1997 and 2013, with numbers generally increasing per year (based on published articles; from Boggi et al., 2014) (5). Among the four techniques, pure laparoscopy gained the highest preference with more than half of the total LPD (51.7%) while the hand-assisted operation had the smallest number, around 0.6%. Not including the hand-assisted LPD, the other three operations obtained similar results with regard to the overall morbidity and mortality. However, in terms of blood loss, operative time and pancreatic fistula rates, pure laparoscopy had preferable results over the other two operations. Meanwhile, robotic-assisted LPD (RA-LPD) was also becoming popular; however, this system is not evenly available throughout the world (8), as the cost for this approach remained high and several limitations were reported for the use of this system such as the risk of malfunction and system collision (9,10), the lack of haptic feedback and the inability to move the patient after the robot has started operating (10), among others. Despite these limitations, performing this RA-LPD improves the dexterity of surgeons and surgical maneuver is easier compared to the open approach. Interestingly, using the data of all four techniques mentioned above (see Table 1), the number of LPD (Figure 1) reported in a more than a year (from January 2012 to June 1st 2013) has exceeded the LPD reported in the last 15 years and is a proof that LPD has quickly matured into an acceptable surgical procedure at least in specialized centers and in the hands of surgeons with highly advanced laparoscopic skills (5).
Full table
Comparison between LPD and the open approach
Asbun and Stauffer (4) have compared the outcomes of patients who have undergone LPD with those patients who have undergone OPD based on morbidity and mortality, in a 6-year period (between 2005 and 2011). According to the results, significant differences were observed in favor of LPD that included shorted intensive care unit (ICU) and hospital stay, lower blood loss and transfusions, and higher retrieval of lymph nodes. Although operative time was statistically longer for LPD, there were no difference in overall complications and pancreas fistula between LPD and OPD. Therefore, Asbun and Stauffer (4) have suggested that LPD is safe and feasible and the outcomes were better than OPD. Aside from this, LPD could also offer an extended long-term survival after the operation (13). However, technical difficulty and complexity of this procedure still remain a limitation (4), and other authors still contend that LPD had no significant advantages over OPD since there were no significant differences in terms of blood loss, morbidity, number of lymph nodes harvested, mortality and R0 resection rate (24), which was not in agreement with more recent reports (13,18,30,31) among others.
Kuroki et al. (31) made a retrospective analysis comparing the outcomes of laparoscopically-assisted pancreaticoduodenectomy (LA-PD) and OPD surgeries among 51 patients (n=20 for LA-PD while n=31 for OPD) with pancreatic and periampullary disease. According to their data, operative time and post-operative complications did not differ significantly between the two groups while blood loss was much less in the LA-PD group. This reduced blood loss in minimally invasive surgeries has also been recognized by other authors (30,37). As such, Kuroki et al. (38) concludes that LA-PD is safe, feasible and has an advantage of less blood loss, as is usually the case in minimally invasive surgeries. With regard to operative time, it has been shown that mean time of operation can be lessens with improved skills. For example, Kim et al. (20) recorded a reduction in mean operation time from 9.8 hrs (for the first 33 patients) to 6.6 hrs (for the last 40 patients). Kendrick et al. (23) also reported a reduction in operative time to 5.3 hrs from the previous 7.7 hrs. Because of these findings, it can also be elicited that LPD can be performed efficiently and safely by experienced and highly skilled surgeons, although the learning curve is steep. Also, standardizing LPD protocols may potentially help shorten LPD operative time (38). However, according to Corcione et al. (21), LPD does not provide significant benefits compared to the open approach but may do in specialized centers with surgeons who have acquired highly advanced skills in LPD.
In another study, Croome et al. (18) evaluated the advantages of total laparoscopic pancreaticoduodenectomy (TLPD) (n=108) over OPD (n=124) for pancreatic ductal adenocarcinoma performed from January 2008 until July 2013. The results showed that after operation, the OPD group stayed longer in the hospital (average: 9 days) compared to the TLPD group (average: 6 days). Moreover, progression-free survival was longer in TLPD compared to the PDC group. In patients administered with adjuvant chemotherapy, median time until commencement of treatment was also shorter in TLPD (48 days, ranging from 17–116 days) compared to OPD (59 days, ranging from 25–302 days) and a significantly smaller proportion of patients in the TLPD group had a delay of more than 56 days. Intraoperative transfusions and delayed gastric emptying occurred less frequently in the TLPD group. In terms of overall survival, there was no significant difference between the two. Based on these results, Croome et al. [2014], has emphasized that the TLPD was not only feasible but also had significant advantages over the traditional open approach. Furthermore, Jacobs and Kamyab [2013] have also evaluated the oncologic outcome of TLPD and based on their experience, complication rates were equivalent or improved in TLPS compared to the traditional Whipple procedure. The patients also had a faster recovery and shorter length of stay and a better quality of life.
Comparison between RA-LPD and OPD
Chalikonda et al. (30) made a comparison between the outcomes of RA-LPD and OPD among 60 patients (n=30 for RA-LPD and n=30 for OPD). Based on their case-matched data, the mean operative time for RA-LPD is longer than OPD while the blood loss and length of stay were decreased in the RA-LPD compared to the OPD. Albeit one perioperative death was experienced in the RA-LPD group that has led to emergent conversion to OPD, the need for re-operation did not differ between the two groups. Chalikonda et al. [2012] has recognized surgical robots as having the potential to overcome some technical difficulties associated with laparoscopy and, with the necessary skills needed to perform such operation aligned with the proper selection of patients, good outcomes are achievable with RA-LPD. The only drawback that was mentioned was the high capital and maintenance costs of RA-LPD plus the added costs associated with longer operative time. Accordingly, the reduced morbidity after RA-LPD made it an acceptable and reasonable surgical approach, for appropriately selected patients (30).
In another study, a comparison was done between RA-LPD and OPD surgeries (Lai et al., 2012) among 87 patients (n=20 for RA-LPD and n=67 for OPD) who underwent either of the two operations from January 2000 to February 2012. The results for RA-LPD were longer operative time, less blood loss and shorter hospital stay, in concurrence with the results reported by Chalikonda et al. (30). Furthermore, there were no statistically significant differences between the two groups in terms of complication and mortality rates and total number of lymph nodes harvested. As such, Lai et al. (33) has recognized the safety and feasibility of RA-LPD, although caution should be carefully observed to evaluate the appropriateness of this procedure for each patient. More recently, Parisi et al. (39), has also recognized the evolution of minimally invasive pancreaticoduodenectomy through robotic technology, suggesting it to be feasible, reproducible and safe.
Recently, Chen et al. (32), has also published a study comparing RA-LPD and OPD among 180 patients (n=60 for RA-LPD and n=120 for OPD) who underwent such operations between January 2012 and December 2013. According to the results, patients who underwent RA-LPD had lesser blood loss, longer but decreasing operative time, resumed bowel movement faster, off-bed return to activity faster and length of hospital stay shorter compared to patients who underwent OPD. Based on mortality, morbidity, and disease-free survival, there were no significant differences between the RA-LPD and OPD groups. Hence, the author suggested that RA-LPS is associated with faster recovery, but it involved a large learning curve for surgeons. Table 1 summarizes the intra- and postoperative outcomes of different studies on LPD.
Modifications of the LPD procedure
More recently, Liu et al. (16) has reported a modification of the LPD procedure. With accumulated substantial experience in laparoscopy, a modified and simpler procedure, called the reverse-“V” approach, was developed to optimize LPD for appropriately selected patients. This modified approach is advantageous as it helps in avoiding pancreatic leakage and also lessens difficulty in the surgical union of tubular parts (anastomosis). The procedure was done in four ports (see Liu et al., 2015, for the detailed procedure) in 21 patients. Based on the results, the median blood loss was less (240 mL) as was the operative time (368 minutes). The reported blood loss and operative time for this study is in fact lower than previous studies (22,40). There was also no perioperative mortality reported. Therefore, LPD using a reverse-“V” approach is safe, which can give good results and can be used in treating localized malignant lesions. Since this surgical procedure is feasible and simple at the same time, further investigations should be continually carried out. However, even though this procedure is simpler compared to the traditional LPD procedure, surgeons attempting should be equipped with advanced skills in pancreatic surgery and laparoscopy to avoid complications (14).
Conclusions
It is clear that benefits of LPD over OPD are relative to the respective skill and experience of the surgeon carrying out the procedure. Therefore, in order to continue the improvement of LPD techniques, it is vital to standardise surgical training and carry out further research to identify which aspects of LPD instruction most efficiently teach surgeons to reduce blood loss, tissue trauma and complications. However, when researching this we must be mindful of the extent that the skill of the surgeon has on the outcome of the operation and the differing abilities of surgeons to learn at different stages of the learning curve. Therefore, a possible avenue to achieve this would be using surgical simulation machines to assess how different instructional methods affect blood loss and trauma incurred in subsequent simulated operations.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare
References
- Joyce D, Morris-Stiff G, Falk GA, et al. Robotic surgery of the pancreas. World J Gastroenterol 2014;20:14726-32. [Crossref] [PubMed]
- Fernández-Cruz L. Distal pancreatic resection: technical differences between open and laparoscopic approaches. HPB (Oxford) 2006;8:49-56. [Crossref] [PubMed]
- Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 1994;8:408-10. [Crossref] [PubMed]
- Asbun HJ, Stauffer JA. Laparoscopic vs open pancreaticoduodenectomy: overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg 2012;215:810-9. [Crossref] [PubMed]
- Boggi U, Amorese G, Vistoli F, et al. Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc 2015;29:9-23. [Crossref] [PubMed]
- Li H, Zhou X, Ying D, et al. Laparoscopic pancreaticoduodenectomy. Hepatobiliary Surg Nutr 2014;3:421-2. [PubMed]
- Anderson B, Karmali S. Laparoscopic resection of pancreatic adenocarcinoma: dream or reality? World J Gastroenterol 2014;20:14255-62. [Crossref] [PubMed]
- Vaessen C. Location of robotic surgical systems worldwide and in France. J Visc Surg 2011;148:e9-11. [Crossref] [PubMed]
- Giulianotti PC, Sbrana F, Bianco FM, et al. Robot-assisted laparoscopic pancreatic surgery: single-surgeon experience. Surg Endosc 2010;24:1646-57. [Crossref] [PubMed]
- Zeh HJ 3rd, Bartlett DL, Moser AJ. Robotic-assisted major pancreatic resection. Adv Surg 2011;45:323-40. [Crossref] [PubMed]
- Jin W, Xu X, Mou Y, et al. Early experience of laparoscopic pancreaticoduodenectomy on 66 cases. Zhonghua Wai Ke Za Zhi 2016;54:84-8. [PubMed]
- Kim EY, Hong TH. Total Laparoscopic Pancreaticoduodenectomy Using a New Technique of Pancreaticojejunostomy with Two Transpancreatic Sutures with Buttresses. J Laparoendosc Adv Surg Tech A 2016;26:133-9. [Crossref] [PubMed]
- Wang M, Zhang H, Wu Z, et al. Laparoscopic pancreaticoduodenectomy: single-surgeon experience. Surg Endosc 2015;29:3783-94. [Crossref] [PubMed]
- Senthilnathan P, Srivatsan Gurumurthy S, Gul SI, et al. Long-term results of laparoscopic pancreaticoduodenectomy for pancreatic and periampullary cancer-experience of 130 cases from a tertiary-care center in South India. J Laparoendosc Adv Surg Tech A 2015;25:295-300. [Crossref] [PubMed]
- Mendoza AS 3rd, Han HS, Yoon YS, et al. Laparoscopy-assisted pancreaticoduodenectomy as minimally invasive surgery for periampullary tumors: a comparison of short-term clinical outcomes of laparoscopy-assisted pancreaticoduodenectomy and open pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci 2015;22:819-24. [Crossref] [PubMed]
- Liu Z, Yu MC, Zhao R, et al. Laparoscopic pancreaticoduodenectomy via a reverse-''V'' approach with four ports: initial experience and perioperative outcomes. World J Gastroenterol 2015;21:1588-94. [Crossref] [PubMed]
- Dokmak S, Ftériche FS, Aussilhou B, et al. Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 2015;220:831-8. [Crossref] [PubMed]
- Croome KP, Farnell MB, Que FG, et al. Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg 2015;19:189-94; discussion 194. [Crossref] [PubMed]
- Lee JS, Han JH, Na GH, et al. Laparoscopic pancreaticoduodenectomy assisted by mini-laparotomy. Surg Laparosc Endosc Percutan Tech 2013;23:e98-102. [Crossref] [PubMed]
- Kim SC, Song KB, Jung YS, et al. Short-term clinical outcomes for 100 consecutive cases of laparoscopic pylorus-preserving pancreatoduodenectomy: improvement with surgical experience. Surg Endosc 2013;27:95-103. [Crossref] [PubMed]
- Corcione F, Pirozzi F, Cuccurullo D, et al. Laparoscopic pancreaticoduodenectomy: experience of 22 cases. Surg Endosc 2013;27:2131-6. [Crossref] [PubMed]
- Ammori BJ, Ayiomamitis GD. Laparoscopic pancreaticoduodenectomy and distal pancreatectomy: a UK experience and a systematic review of the literature. Surg Endosc 2011;25:2084-99. [Crossref] [PubMed]
- Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: feasibility and outcome in an early experience. Arch Surg 2010;145:19-23. [Crossref] [PubMed]
- Zureikat AH, Breaux JA, Steel JL, et al. Can laparoscopic pancreaticoduodenectomy be safely implemented? J Gastrointest Surg 2011;15:1151-7. [Crossref] [PubMed]
- Song KB, Kim SC, Hwang DW, et al. Matched Case-Control Analysis Comparing Laparoscopic and Open Pylorus-preserving Pancreaticoduodenectomy in Patients With Periampullary Tumors. Ann Surg 2015;262:146-55. [Crossref] [PubMed]
- Wellner UF, Küsters S, Sick O, et al. Hybrid laparoscopic versus open pylorus-preserving pancreatoduodenectomy: retrospective matched case comparison in 80 patients. Langenbecks Arch Surg 2014;399:849-56. [Crossref] [PubMed]
- Gumbs AA, Croner R, Rodriguez A, et al. 200 consecutive laparoscopic pancreatic resections performed with a robotically controlled laparoscope holder. Surg Endosc 2013;27:3781-91. [Crossref] [PubMed]
- Paniccia A, Schulick RD, Edil BH. Total Laparoscopic Pancreaticoduodenectomy: A Single-Institutional Experience. Ann Surg Oncol 2015;22:4380-1. [Crossref] [PubMed]
- Tan CL, Zhang H, Peng B, et al. Outcome and costs of laparoscopic pancreaticoduodenectomy during the initial learning curve vs laparotomy. World J Gastroenterol 2015;21:5311-9. [Crossref] [PubMed]
- Chalikonda S, Aguilar-Saavedra JR, Walsh RM. Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc 2012;26:2397-402. [Crossref] [PubMed]
- Kuroki T, Adachi T, Okamoto T, et al. A non-randomized comparative study of laparoscopy-assisted pancreaticoduodenectomy and open pancreaticoduodenectomy. Hepatogastroenterology 2012;59:570-3. [Crossref] [PubMed]
- Chen S, Chen JZ, Zhan Q, et al. Robot-assisted laparoscopic versus open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc 2015;29:3698-711. [Crossref] [PubMed]
- Lai EC, Yang GP, Tang CN. Robot-assisted laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy--a comparative study. Int J Surg 2012;10:475-9. [Crossref] [PubMed]
- Suzuki O, Kondo S, Hirano S, et al. Laparoscopic pancreaticoduodenectomy combined with minilaparotomy. Surg Today 2012;42:509-13. [Crossref] [PubMed]
- Bao PQ, Mazirka PO, Watkins KT. Retrospective comparison of robot-assisted minimally invasive versus open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg 2014;18:682-9. [Crossref] [PubMed]
- Jacobs MJ, Kamyab A. Total laparoscopic pancreaticoduodenectomy. JSLS 2013;17:188-93. [Crossref] [PubMed]
- Jayaraman S, Gonen M, Brennan MF, et al. Laparoscopic distal pancreatectomy: evolution of a technique at a single institution. J Am Coll Surg 2010;211:503-9. [Crossref] [PubMed]
- Kuroki T, Eguchi S. Laparoscopic distal pancreatosplenectomy for pancreatic ductal adenocarcinoma. Surg Today 2015;45:808-12. [Crossref] [PubMed]
- Parisi A, Desiderio J, Trastulli S, et al. Robotic pancreaticoduodenectomy in a case of duodenal gastrointestinal stromal tumor. World J Surg Oncol 2014;12:372. [Crossref] [PubMed]
- Cai X, Wang Y, Yu H, et al. Completed laparoscopic pancreaticoduodenectomy. Surg Laparosc Endosc Percutan Tech 2008;18:404-6. [Crossref] [PubMed]