Editor’s note:
The special column “Statistics in Oncology Clinical Trials” is dedicated to providing state-of-the-art review or perspectives of statistical issues in oncology clinical trials. Our Chairs for the column are Dr. Daniel Sargent and Dr. Qian Shi, Division of Biomedical Statistics and Informatics, Mayo Clinic, Rochester, MN, USA. The column is expected to convey statistical knowledge which is essential to trial design, conduct, and monitoring for a wide range of researchers in the oncology area. Through illustrations of the basic concepts, discussions of current debates and concerns in the literature, and highlights of evolutionary new developments, we are hoping to engage and strengthen the collaboration between statisticians and oncologists for conducting innovative clinical trials. Please follow the column and enjoy.
Findings from the Adjuvant Colon Cancer End Points (ACCENT) Collaborative Group: the power of pooled individual patient data from multiple clinical trials
Introduction
Individual patient data from randomized clinical trials are often desirable to study key clinical questions such as drivers of patient prognosis, effects of specific disease factors on patient outcomes, and markers of differential response to treatment. Advantages inherent to analyses based on clinical trial data include prospectively defined standards for consistent data collection, uniformity of the patient population via a trial’s inclusion/exclusion criteria, stricter adherence of trial patients to protocol and treatment procedures, and consistent and thorough follow-up of the patients enrolled. These features of individual patient data from clinical trials allow corresponding clinical questions of interest to be analyzed more clearly and definitively, even as cancer clinical trials are becoming increasingly sophisticated in design and comprehensive in data collection, often including tumor genomics and biomarkers.
However, as cancer is increasingly understood to be a heterogeneous disease even within common cancer types such as colorectal cancer, late phase clinical trials are likely to become smaller in order to increase efficiency and reduce costs. At the same time, the generalizable knowledge that may be gleaned from even the largest clinical trial remains limited, not only by sample size but also by geographic location, narrow focus on particular treatments, or other built-in constraints. Fortunately, multiple clinical trials with similar patient populations and therapeutic objectives are often conducted in parallel by different groups, sometimes internationally. With carefully orchestrated efforts and international collaborations such as those initiated and maintained by the Adjuvant Colon Cancer Endpoints (ACCENT) Group (Figure 1), the information contained in multiple similar studies conducted either in sequence or in parallel may be combined and leveraged to answer important disease questions that no single trial can address in isolation.
Over the last 15 years, the ACCENT Group has created a database of 27 randomized phase III clinical trials in early stage colon cancer, including individual patient data from more than 40,000 stage II and III patients enrolled to the trials from 1977 through 2009 (1-5). The database itself includes patient demographics and disease characteristics, treatment data, biomarkers (for selected studies), adverse events, as well as lengthy and validated recurrence and survival follow-up for all patients. Trials contained in ACCENT were selected for both their quality and importance, with inclusion of pivotal trials that have changed the practice of colon cancer treatment over the last 25 years. This collaboration has notably served as a prototype for the construction of databases in other disease settings including advanced colorectal cancer (6), extensive-stage small cell lung cancer (7), and follicular lymphoma (8), among others.
In this review, we provide a brief overview of the collaborative origins of ACCENT, including construction of the database and principles governing its use. We then highlight selected notable research outcomes of the ACCENT database published to date, and indicate future research endeavors.
History and principles of the ACCENT database
History of ACCENT
The ACCENT group was formed organically over several years in response to scientific questions in colon cancer research requiring pooled analyses of clinical trials to address. Prior to the birth of ACCENT, the IMPACT group combined data from 3 trials testing 5-FU with leucovorin vs. surgery-alone control in patients with stage II and III disease in order to construct a more powerful analysis of the benefit of adjuvant chemotherapy (9). Individual patient data from these 3 trials were subsequently combined with data from two additional trials to conduct an analysis of the benefit of adjuvant chemotherapy specifically within the population of stage II patients (10), and later, these 5 trials were pooled with 2 additional North Central Cancer Treatment Group (NCCTG) trials to examine the benefit of adjuvant therapy in elderly patients (11).
In 2003, the ACCENT collaborative group was formally created following a meeting in Paris, France where the potential surrogacy of disease-free survival (DFS) for overall survival (OS) was discussed. At this juncture, 6 more trials from NCCTG and the National Surgical Adjuvant Breast and Bowel Project (NSABP) were contributed to ACCENT, followed by 5 trials from other groups, resulting in ACCENT’s initial set of 18 trials studying adjuvant chemotherapy (1) (Table 1). In 2009, the database was updated with individual patient data from 6 newly mature trials testing oxaliplatin or irinotecan added to 5-FU/LV or oral fluoropyrimidines (2), and in more recent years, data from N0147, NSABP C-08, and the XELOXA trial have been added as well (3-5).
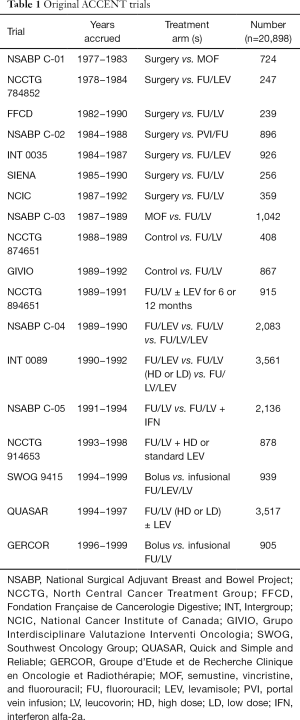
Full table
ACCENT principles
Soliciting, collecting, combining, and maintaining individual patient data from multiple clinical trials requires considerable time, effort, and organization, as discussed previously by our group (12). For ACCENT, principles governing use of the pooled data include open participation by contributing investigators, internal and external scientific peer review, collaborative authorship, and unanimous support for proposed research projects to move forward. Specifically, any contributing or participating person or group may submit a formal research proposal that may possibly be addressed by the data contained in the ACCENT database. Requests are circulated to all participating ACCENT investigators including clinical oncologists and biostatisticians, who together assess plausibility, feasibility, design, rationale, and likely impact of the proposed research. Each ACCENT trial’s lead investigator may choose to withdraw his or her trial’s data from use within a specific project (to date, this has not occurred) or voice general scientific objections. Once critical consensus is reached for a given proposal, members interested in the proposal’s topic form a core authorship group, combining required resources and attention to move the project to completion. Successful endeavors yield peer-reviewed manuscripts published in high impact scientific journals with authorship reflecting comprehensive scientific, statistical, and original data contributions.
ACCENT research and publications
Over the last 15 years, the ACCENT collaboration has helped to address many important scientific questions in early stage colon cancer by pooling individual patient data from its trials. Here, we provide a high-level review of published ACCENT analyses to date, including and subsequently expanding upon those described previously (12).
Adjuvant chemotherapy in elderly patients
Whether elderly colon cancer patients benefit from treatment with adjuvant chemotherapy following curative resection has been poorly understood, with limited data obscuring or precluding practical guidelines. The main limitation of existing data from clinical trials is the relatively low proportion of elderly patients within any given study, which prohibits meaningful single-trial inference. Frequently, elderly patients have been excluded from clinical trials by design or not offered adjuvant chemotherapy due to perceived or health-related risks, exacerbating the problem of clinical study of this patient population. To address the question of whether the broadly established benefit of 5-FU based regimens was specifically applicable to elderly patients, in 2001, Sargent et al. published a pooled analysis of 7 adjuvant therapy trials (GIVIO, NCIC-CTG, FFCD and four NCCTG studies) in which patients were randomized to surgical resection followed by adjuvant chemotherapy versus surgery alone (11). When therapeutic benefit from chemotherapy was analyzed within patients younger versus older than 70 years of age, it was found that chemotherapy benefited elderly patients (those 70 years or older) to the same extent as younger patients.
More than 10 years later in 2013, McCleary et al. performed a similar analysis of the benefit of oral 5-FU or 5-FU with irinotecan or oxaliplatin versus intravenous fluoropyrimidines alone in elderly (age 70+) vs. younger (age <70) patients, with this analysis based on more than 12,000 patients from 7 newer trials containing modern therapies in their experimental arms (13). The authors reported that while no statistically significant interactions between treatment and dichotomized age were found in regression models to support differential treatment effects on TTR, DFS, or OS, some empirical treatment effects within the two age groups suggested a limited benefit of oxaliplatin in elderly patients. Treatment effects were similar between oral and intravenous 5-FU regardless of age, further suggesting the two administrations could be regarded as exchangeable in terms of efficacy.
Early prognostic and predictive models
In 2004, Gill et al. used 3,302 patients from the same 7 adjuvant trials as those analyzed by Sargent et al. (11) to determine whether several different patient and disease factors were prognostic for 5-year DFS or 5-year OS, or predictive of benefit from FU-based regimens (14). It was found that nodal status, tumor stage, and grade were independently prognostic for both DFS and OS, while age was significant only for OS. Treatment benefit was consistent across age, sex, tumor location and stage, and tumor grade, while a significant stage-by-treatment interaction indicated greater benefit of adjuvant therapy for stage III than stage II patients. These early clinical prediction models or “nomograms” were then implemented as calculators (collectively named Numeracy) for clinical use on Mayo Clinic’s website; in 2014, they were replaced by updated calculators derived from ACCENT as described later in this section.
DFS as surrogate for OS
As adjuvant therapy has become increasingly effective, and post-recurrent survival has also been lengthened, the need for an earlier endpoint for adjuvant therapy finally became clear. In 2003, the ACCENT group pursued an analysis to examine whether DFS could be formally validated as a surrogate endpoint for OS and then subsequently replace OS as a primary endpoint in future adjuvant colon cancer trials. In 2005, ACCENT confirmed that DFS with median of 3-year follow-up was an appropriate surrogate endpoint for OS with median of 5-year follow-up, according to a robust set of multi-trial surrogacy analyses that remain the standard analytic approach today (1,15).
In 2007, Sargent et al. expanded their 2005 results by investigating whether DFS with 1- or 2-year follow-up could serve as potential surrogates for OS with 5-year follow-up, in addition to quantifying the dependency of DFS’s surrogacy on stage of disease (16). Using the 18 original ACCENT trials, the authors found that DFS with less than 3-year follow-up proved to be less accurate in predicting OS than the previously validated surrogate endpoint of DFS with 3-year follow up, and furthermore, the DFS-OS surrogacy association was stronger for stage III than stage II disease. The latter finding suggested that use of DFS as a surrogate for OS is most appropriate in trials comprised mostly or entirely of stage III patients.
Survival following recurrence
By the early 2000s, it was noted that the average time from patient recurrence to death had lengthened, which was often attributed to availability of post-recurrence regimens and other therapeutic options. This interest in post-recurrence survival prompted the ACCENT group to identify specific factors influencing length of survival following recurrence. In 2008, O’Connell and colleagues utilized a subset of approximately 33% of ACCENT patients with documented recurrence to investigate the impact of patient age, time to initial recurrence, disease stage (II vs. III), receipt of adjuvant treatment (FU-based vs. surgery alone), and year of enrollment on length of subsequent survival (17). All of the factors investigated were significant predictors of post-recurrence survival with the interesting biologic findings that patients with initial stage II disease live longer after recurrence than patients with initial stage III disease, suggests a different disease biology by stage.
In a parallel analysis involving newer therapies that had been found to prolong survival time beyond recurrence, de Gramont et al. used patient-level data from ACCENT to simulate the impact of longer survival post-recurrence on the strength of surrogacy of DFS for OS (18). These authors found that lengthened post-recurrence survival weakens the previously validated surrogacy relationship, while surrogacy of DFS strengthened with increased (>5 years) follow-up on OS, therefore maintaining support for the use of DFS as a primary endpoint in modern adjuvant chemotherapy trials.
Evidence for cure by adjuvant chemotherapy
By 2009, ACCENT collaborators had thoroughly studied relationships between disease recurrence and OS and the impact of adjuvant chemotherapy, but these studies were mostly limited to 5-year patient follow-up. For this reason, longer-term outcomes and implications in colon cancer had not yet been explored. Once a median of 8-year follow-up was reached for the original ACCENT trials, Sargent et al. confirmed that the previously identified survival benefit attributable to adjuvant chemotherapy was indeed sustained over 8 years of available patient follow-up, with the recurrence risk of patients who received chemotherapy never exceeding that of patients treated with surgery alone (19). Based on this fact, the authors concluded that a subset of chemotherapy-treated patients in ACCENT were in fact cured of their disease, with recurrence rates declining to less than 1% per year for patients followed beyond 8 years. However, in a time-dependent analysis of the treatment effect on DFS of adjuvant chemotherapy versus surgery alone, it was found that benefit from chemotherapy (as gauged by sustained reduction in the hazard of DFS over time) was limited to the first 2-year post-randomization, after which the risk curves between pooled treatment arms were similar. The authors interpreted this finding to suggest that adjuvant therapy’s primary benefit is a highly significant reduction of the risk of recurrence in the first 2 years following surgery.
Evaluation of DFS as endpoint for trials of oral 5-FU or modern combination adjuvant therapies
In the late 2000s, recently completed clinical trials of new adjuvant chemotherapies including oral fluoropyrimidines and combination therapies (5-FU plus oxaliplatin or irinotecan) began to reach mature patient follow-up. In 2009, the ACCENT database acquired 6 of these trials (2), as listed in Table 2. The additional individual patient data these trials provided would not only aid in answering important disease-specific questions with greater power, but would also be examined to learn whether previously published findings under the former treatment paradigm would persist with modern trials and treatments. In 2011, Sargent et al. re-evaluated the surrogacy of DFS for OS among the new ACCENT trials and found the strength of the surrogacy relationship to be somewhat diminished, especially for stage II patients (2). The authors maintained that while DFS remained an appropriate endpoint for trials including patients with stage III disease, at least 6-year follow-up should be obtained to assess OS benefit due to improved diagnosis, staging, and treatment standards.
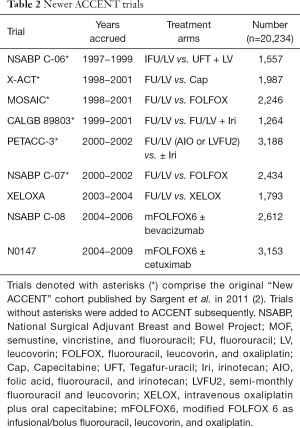
Full table
Racial disparities in colon cancer prognosis
In 2011, in response to other published reports of black colon cancer patients having worse survival than white patients, Yothers et al. performed a pooled analysis of randomized clinical trials contained in ACCENT to determine whether disparities persisted when both groups received identical treatment assignments in clinical trials (20). Unfortunately, the authors discovered decreased recurrence-free survival and OS for black relative to white patients, with worse survival among blacks also observed in subsets defined by sex, age, and stage of disease. In contrast, the time to recurrence (TTR) did not differ according to race, suggesting the disease process and corresponding risk of recurrence is similar for blacks and whites, but black patients likely experience poorer post-surgical survival due to other factors.
Treatment benefit and toxicity in young vs. old patients
Until recently, little was understood regarding patterns of treatment benefit or excess adverse events associated with adjuvant chemotherapy in very young patients. In 2012, Hubbard et al. pooled patient-level data from the 24 trials then contained in ACCENT to examine efficacy and toxicity outcomes by age, with young patients defined by two thresholds: those with age less than 40 years (5.2%) or age less than 50 years (17.3%) (21). In this study, regardless of the threshold chosen, very young patients were found not to differ from older patients in terms of TTR, but younger patients experienced improved OS and DFS relative to older patients. Among the 9 trials where significant efficacy was demonstrated for the experimental arm, the DFS benefit was similar by age group. Likelihood of specific adverse events also differed by age, with younger patients experiencing less leukopenia and stomatitis, but more frequent nausea and vomiting. This analysis serves as a key example of the power of the ACCENT database: when the population of interest (in this case, very young patients with colon cancer) comprises only a small percentage of those patients enrolled to any single trial, the answers to questions such as these can only be meaningfully obtained by combining such patients across many similar trials.
Oxaliplatin benefit in trial vs. general populations
By 2012, the benefit of 5-FU plus oxaliplatin regimens (e.g., FOLFOX) in the treatment of early stage colon cancer had been well established; however, these promising results were demonstrated from the relatively younger, healthier population of patients eligible for participation in clinical trials. It remained unclear whether these benefits would extend to a more representative patient population with comorbidities or more compromised disease. To investigate this, Dr. Sanoff and colleagues pooled outcomes from patients in ACCENT and compared them against those obtained from the Surveillance, Epidemiology, and End Results (SEER) registry linked to Medicare claims (SEER-Medicare), the New York State Cancer Registry (NYSCR), the National Comprehensive Cancer Network (NCCN) Outcomes Database, and the Cancer Care Outcomes Research & Surveillance Consortium (CanCORS). This analysis supported the conclusion that the added benefit of oxaliplatin as part of a fluorouracil-based adjuvant chemotherapy regimen extended to the general population, including older patients, minorities, and those with a higher burden of comorbidities (22).
Body mass index (BMI) as a prognostic factor in colon cancer
While high BMI has been well established as a strong risk factor in development of colon cancer, until recently, the prognostic or predictive impact of BMI at time of treatment initiation on the outcomes of colon cancer patients treated with adjuvant therapy had not been explored. In 2012, Dr. Sinicrope and other ACCENT collaborators performed a pooled analysis of the impact of baseline patient BMI on TTR, DFS, and OS (23). Of the 25,291 patients examined, both underweight and obese patients showed worse OS than either normal weight or overweight patients; however, this pattern only reached statistical significance for men. Additionally, men with severe (class 2 or 3) obesity at randomization demonstrated significantly shorter DFS than normal-weight men, while both men and women with underweight BMI showed reduced TTR and DFS. Of note, BMI did not differentially predict benefit from adjuvant therapy.
Patient sex as a prognostic factor in colon cancer
In 2013, Cheung et al. pooled 33,345 patients from 24 trials contained in the ACCENT database to examine whether male and female patients experienced differing TTR, DFS, or OS, and whether any other factors such as treatment, age, or stage of disease mediated a potential sex effect on patient outcomes (24). It was found that males had slightly worse outcomes than females overall and after adjustment for patient and disease characteristics, but that patient sex was not a predictive factor of treatment efficacy in general or within any patient subgroup explored. Among elderly patients, worse outcomes for men than women became more pronounced, but the prognostic value of patient sex remained similar within patients with stage II and III disease.
Evidence of stage migration from 1978−1995 to 1996−2007
Following recognized improvements in treatment options, disease surveillance, and availability of subsequent chemotherapies for early stage colon cancer patients, it was hypothesized that patient outcomes had generally improved in recent decades. To examine this, Shi et al. pooled individual patient data from 18,449 patients from 21 clinical trials contained in ACCENT to evaluate potential shifts in TTR, time from recurrence to death (TRD), and OS from patients enrolled during time period 1978−1995 to those enrolled in 1996 and beyond (25). While lower recurrence rates within the first 3-year post-randomization were noted for stage II patients enrolled to more recent versus older trials, this improvement was not noted for patients with stage III disease enrolled to newer trials. Improved TRD and OS were described for patients from recent trials who received modern adjuvant chemotherapy, overall and within each disease stage, with the lymph node ratio (number of positive nodes to number of nodes examined) also decreasing over time. The authors concluded that the longer TTR observed for stage II patients in newer trials who were randomized to receive identical treatments as stage II patients from older trials suggested a stage migration, or apparent improvement in outcomes of stage II patients over time that can be primarily attributed to the advent of modern staging guidelines (such as evaluating at least 12 lymph nodes for positivity).
ACCENT-based web calculators for recurrence and survival in stage III disease
As described earlier, the initial set of trials contained in the ACCENT database was used to construct an online calculator, Numeracy, that provided patient-specific recurrence and survival estimates given treatment (surgery alone versus fluorouracil-based adjuvant therapy) and a limited set of demographic and disease characteristics (13). In 2014, Renfro et al. created an updated prognostic calculator for stage III colon cancer patients to replace the Numeracy calculator on the Mayo Clinic website, using a more modern set of trials from the ACCENT database including those that enrolled patients since 1990 and trials containing treatment regimens with oxaliplatin (26). The new ACCENT-based calculators input a patient’s age, sex, BMI, race, ECOG/WHO performance status, tumor stage, tumor grade, tumor location, number of lymph nodes examined and number positive, and planned chemotherapy approach (none vs. 5-FU-based regimens vs. FOLFOX) and return patient-specific estimates of the probabilities of recurrence-free status and survival at 5-year post-resection. The new calculator demonstrated both strong internal validity and external validity when assessed using patients from independent trial NSABP C-08, and further demonstrated predictive superiority to Numeracy. Clinicians may access the ACCENT calculator here: http://www.mayoclinic.org/medical-professionals/cancer-prediction-tools/colon-cancer.
Survival following colon cancer: comparison vs. general population survival
By this point in time, it was established that 5-FU-based chemotherapy—particularly in combination with oxaliplatin—may be curative in some patients with early stage colon cancer. However, it was not well understood how a treated patient might fare in the long term compared to an individual who had never been diagnosed with colon cancer. To make this comparison more formal, Renfro et al. constructed a hypothetical non-cancer-related survival trajectory for each of the 32,745 patients contained in the ACCENT database using the patients’ age, sex, year of treatment initiation for colon cancer, and official life tables from the 41 countries where the patients had enrolled to their respective trials (27). Comparisons between actual ACCENT patient survival and predicted matched general survival were then made overall and within subgroups of patients defined by stage of disease, treatment, and other factors. These comparisons were made at randomization and conditional on survival to subsequent annual landmarks up to 5 years. The authors found that within most cohorts, long-term survival of colon cancer patients remained statistically worse than their matched general population, although stage II patients, those treated with oxaliplatin, elderly patients, and patients without recurrence after 5 years could reasonably expect to achieve a projected survival similar to the overall matched general population.
Determinants of early mortality among early stage colon cancer patients
In 2016, Cheung et al. used the ACCENT database to investigate factors associated with early mortality among 37,568 patients from 25 clinical trials, where early mortality was defined as death from any cause within the first 6-month post-randomization (28). The authors found that overall, the rate of early mortality was quite low (1.4% by 6 months), with 40% of those patients who died having documented disease recurrence prior to death. Patients with disease recurrence demonstrated an 82-fold increased risk of early mortality compared to patients without recurrence, with advanced age, male sex, poorer PS, and an increased ratio of the number of positive lymph nodes to nodes examined associated with early mortality to a far lesser degree. Cheung et al. further used ACCENT to develop and validate a clinical nomogram to predict an individual patient’s risk of early mortality given his or her demographic and disease characteristics.
Factors impacting time-dependent recurrence risk and benefit from oxaliplatin
While Sargent et al. 2009 (18) examined the time-dependence of the treatment benefit of chemotherapy versus surgery alone, subsequently, the time-dependence of the benefit of oxaliplatin addition to chemotherapy had not been investigated. In 2016, Shah et al. (29) demonstrated that oxaliplatin significantly reduces the risk of recurrence within the first 14-month post-treatment for patients with stage II colon cancer and significantly reduces risk for up to 4 years for patients with stage III disease. Furthermore, the risk of death from stage III colon cancer was significantly reduced from 2- to 6-year post-treatment, with no difference in the timing of outcomes between treatment groups (i.e., addition of oxaliplatin prevents rather than postpones disease recurrence). The authors’ intuitively visual presentation of how oxaliplatin dramatically reduces the risk of recurrence and/or death over time, both overall and within subgroups of patients defined by tumor or nodal burden, will collectively aid our understanding of the time course of colon cancer and facilitate risk/benefit assessments regarding addition of oxaliplatin to chemotherapy for individual patients.
Non-clinical uses of the ACCENT database and future directions
ACCENT motivation of improved statistical methods
In addition to facilitating numerous large-scale prognostic, predictive, and therapeutic evaluations in early stage colon cancer, the ACCENT database has served as an important resource for developing and testing novel statistical methods or unconventional analysis techniques. While non-parametric (e.g., Kaplan-Meier) and semi-parametric (e.g., Cox proportional hazards) modeling are ubiquitous in the medical literature for analysis of time-to-event endpoints, it is also established that use of parametric (e.g., exponential or Weibull) models for time-to-event outcomes may lend greater precision to estimation of regression effects when the chosen parametric models are truly a good fit to the data of interest. To this end, Chapman and colleagues (30) investigated whether the log-normal distribution provides estimation performance superior to semi- and non-parametric models for the endpoints TTR, DFS, or OS in the setting of early stage colon cancer. The authors concluded that for a subset of ACCENT patients, the log-normal distribution demonstrated limited improved performance over Cox proportional hazards modeling.
Other statistical methodology investigations have flourished with access to the ACCENT database, where assessment of complex multi-trial surrogate endpoint evaluation techniques and novel adaptive clinical trial designs have been successfully motivated by application to actual data. In 2011, Shi et al. used the ACCENT database to perform a simulation and data-driven comparative assessment of trial-level surrogacy evaluation methodologies present in the literature to date, revealing trial features now understood to be associated with increased bias or variability in surrogacy assessments (31). Subsequently, Renfro et al. used the ACCENT database to propose a Bayesian approach for trial-level surrogacy evaluation that takes estimation error of trial-specific treatment effects into account (32). Renfro and colleagues also proposed an improved copula-based approach to estimation of patient-level and trial-level surrogacy (33) and an exploration of the impact of performing multi-trial surrogacy evaluations on trial sub-units (such as centers within trials) when a large number of trials are not available for analysis (34). A Bayesian adaptive trial design for a newly validated surrogate endpoint has also been developed and demonstrated using the trials from ACCENT (35).
Ongoing ACCENT projects and new trial additions
To date, the ACCENT group has continuously accumulated valuable clinical, treatment, outcome, and genetic markers data from pivotal trials over an extended period of time now exceeding 35 years. Our group is currently in the process of acquiring patient-level data from several new adjuvant therapy trials, including (we expect) AVANT (36), PETACC8 (37), QUASAR2 (38), and VICTOR (39). Moreover, several new ACCENT projects are ongoing, which we will describe here in brief.
In one project in progress, the ACCENT database is being used to characterize the incidence of specific adverse events by type of adjuvant therapy and to determine whether frequency or intensity of toxicities is associated with patient or disease characteristics such as age, sex, performance status, and stage of disease, or whether certain patterns of toxicities are differentially associated with patient prognosis. In another ongoing project, the performance of the ACCENT-based prognostic calculator developed by Renfro et al. (26) currently hosted on Mayo Clinic’s website will be compared with another prognostic calculator maintained by Memorial Sloan Kettering Cancer Center (40) using patient-level data from a population registry and independent, newly-acquired clinical trials in ACCENT not originally used to construct the ACCENT-based calculator. From this collaboration between the ACCENT and MSKCC groups, the overall performance of each calculator in terms of predicted versus actual patient outcomes will be reported, and differences in the performance between the two calculators within subgroups defined by patient and disease variables will be described. ACCENT projects planned for the near future include an update to the current ACCENT-based prognostic calculator to incorporate more recent trials and tumor biomarkers such as microsatellite instability (MSI) or DNA mismatch-repair (MMR), KRAS, and BRAF, among other endeavors.
Conclusions
Since its establishment in 2001, collaborations by the ACCENT group have played a significant role in improving the efficiency of trial conduct in stage II and III colon cancer and have aided our collective understanding of disease prognosis and time course of modern oxaliplatin-based therapies. As newer trials are added to the ACCENT database and new scientific questions arise, the power of harnessed by pooling individual patient data from dozens of clinical trials will continue to yield additional clinical understanding and tools to enhance the treatment of patients. Future opportunities within ACCENT include additional refinement of optimal endpoints for use in clinical trials within patient sub-populations (such as biomarker-defined groups), updated understanding of the mechanisms by which treatment delays or impedes colon cancer recurrence, and identification of factors that influence and prolong post-recurrence survival. Ultimately, the insights gained by thoughtful examination of this collection of clinical trials will facilitate timely assessment of new adjuvant therapies, with the overall objective of significantly improved outcomes for patients with colon cancer.
Acknowledgements
Funding: This publication was supported by CTSA Grant Number KL2 TR000136 from the National Center for Advancing Translational Science (NCATS). Funding was also provided by R01 CA174779/CA/NCI NIH HHS/United States.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
References
- Sargent DJ, Wieand HS, Haller DG, et al. Disease-free survival versus overall survival as a primary end point for adjuvant colon cancer studies: individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol 2005;23:8664-70. [Crossref] [PubMed]
- Sargent D, Shi Q, Yothers G, et al. Two or three year disease-free survival (DFS) as a primary end-point in stage III adjuvant colon cancer trials with fluoropyrimidines with or without oxaliplatin or irinotecan: data from 12,676 patients from MOSAIC, X-ACT, PETACC-3, C-06, C-07 and C89803. Eur J Cancer 2011;47:990-6. [Crossref] [PubMed]
- Alberts SR, Sargent DJ, Nair S, et al. Effect of oxaliplatin, fluorouracil, and leucovorin with or without cetuximab on survival among patients with resected stage III colon cancer: a randomized trial. JAMA 2012;307:1383-93. [Crossref] [PubMed]
- Allegra CJ, Yothers G, O'Connell MJ, et al. Phase III trial assessing bevacizumab in stages II and III carcinoma of the colon: results of NSABP protocol C-08. J Clin Oncol 2011;29:11-6. [Crossref] [PubMed]
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465-71. [Crossref] [PubMed]
- Shi Q, de Gramont A, Grothey A, et al. Individual patient data analysis of progression-free survival versus overall survival as a first-line end point for metastatic colorectal cancer in modern randomized trials: findings from the analysis and research in cancers of the digestive system database. J Clin Oncol 2015;33:22-8. [Crossref] [PubMed]
- Foster NR, Renfro LA, Schild SE, et al. Multitrial Evaluation of Progression-Free Survival as a Surrogate End Point for Overall Survival in First-Line Extensive-Stage Small-Cell Lung Cancer. J Thorac Oncol 2015;10:1099-106. [Crossref] [PubMed]
- Sargent DJ, Shi Q, De Boudout S, et al. Evaluation of complete response rate at 30 months (CR30) as a surrogate for progression-free survival (PFS) in first-line follicular lymphoma (FL) studies: Results from the prospectively specified Follicular Lymphoma Analysis of Surrogacy Hypothesis (FLASH) analysis with individual patient data (IPD) of 3,837 patients (pts). J Clin Oncol 2015;33:abstr 8504.
- Efficacy of adjuvant fluorouracil and folinic acid in colon cancer. International Multicentre Pooled Analysis of Colon Cancer Trials (IMPACT) investigators. Lancet. 1995;345:939-44. [Crossref] [PubMed]
- Efficacy of adjuvant fluorouracil and folinic acid in B2 colon cancer. International Multicentre Pooled Analysis of B2 Colon Cancer Trials (IMPACT B2) Investigators. J Clin Oncol 1999;17:1356-63. [PubMed]
- Sargent DJ, Goldberg RM, Jacobson SD, et al. A pooled analysis of adjuvant chemotherapy for resected colon cancer in elderly patients. N Engl J Med 2001;345:1091-7. [Crossref] [PubMed]
- Renfro LA, Shi Q, Sargent DJ. Mining the ACCENT database: a review and update. Chin Clin Oncol 2013;2:18. [PubMed]
- McCleary NJ, Meyerhardt JA, Green E, et al. Impact of age on the efficacy of newer adjuvant therapies in patients with stage II/III colon cancer: findings from the ACCENT database. J Clin Oncol 2013;31:2600-6. [Crossref] [PubMed]
- Gill S, Loprinzi CL, Sargent DJ, et al. Pooled analysis of fluorouracil-based adjuvant therapy for stage II and III colon cancer: who benefits and by how much? J Clin Oncol 2004;22:1797-806. [Crossref] [PubMed]
- Burzykowski T, Molenberghs G, Buyse M, et al. Validation of surrogate end points in multiple randomized clinical trials with failure time end points. Appl Stat 2001;50:405-22. [Crossref]
- Sargent DJ, Patiyil S, Yothers G, et al. End points for colon cancer adjuvant trials: observations and recommendations based on individual patient data from 20,898 patients enrolled onto 18 randomized trials from the ACCENT Group. J Clin Oncol 2007;25:4569-74. [Crossref] [PubMed]
- O'Connell MJ, Campbell ME, Goldberg RM, et al. Survival following recurrence in stage II and III colon cancer: findings from the ACCENT data set. J Clin Oncol 2008;26:2336-41. [Crossref] [PubMed]
- de Gramont A, Hubbard J, Shi Q, et al. Association between disease-free survival and overall survival when survival is prolonged after recurrence in patients receiving cytotoxic adjuvant therapy for colon cancer: simulations based on the 20,800 patient ACCENT data set. J Clin Oncol 2010;28:460-5. [Crossref] [PubMed]
- Sargent D, Sobrero A, Grothey A, et al. Evidence for cure by adjuvant therapy in colon cancer: observations based on individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol 2009;27:872-7. [Crossref] [PubMed]
- Yothers G, Sargent DJ, Wolmark N, et al. Outcomes among black patients with stage II and III colon cancer receiving chemotherapy: an analysis of ACCENT adjuvant trials. J Natl Cancer Inst 2011;103:1498-506. [Crossref] [PubMed]
- Hubbard J, Thomas DM, Yothers G, et al. Benefits and adverse events in younger versus older patients receiving adjuvant chemotherapy for colon cancer: findings from the Adjuvant Colon Cancer Endpoints data set. J Clin Oncol 2012;30:2334-9. [Crossref] [PubMed]
- Sanoff HK, Carpenter WR, Martin CF, et al. Comparative effectiveness of oxaliplatin vs non-oxaliplatin-containing adjuvant chemotherapy for stage III colon cancer. J Natl Cancer Inst 2012;104:211-27. [Crossref] [PubMed]
- Sinicrope FA, Foster NR, Yothers G, et al. Body mass index at diagnosis and survival among colon cancer patients enrolled in clinical trials of adjuvant chemotherapy. Cancer 2013;119:1528-36. [Crossref] [PubMed]
- Cheung WY, Shi Q, O'Connell M, et al. The predictive and prognostic value of sex in early-stage colon cancer: a pooled analysis of 33,345 patients from the ACCENT database. Clin Colorectal Cancer 2013;12:179-87. [Crossref] [PubMed]
- Shi Q, Andre T, Grothey A, et al. Comparison of outcomes after fluorouracil-based adjuvant therapy for stages II and III colon cancer between 1978 to 1995 and 1996 to 2007: evidence of stage migration from the ACCENT database. J Clin Oncol 2013;31:3656-63. [Crossref] [PubMed]
- Renfro LA, Grothey A, Xue Y, et al. ACCENT-based web calculators to predict recurrence and overall survival in stage III colon cancer. J Natl Cancer Inst 2014.106. [PubMed]
- Renfro LA, Grothey A, Kerr D, et al. Survival following early-stage colon cancer: an ACCENT-based comparison of patients versus a matched international general population†. Ann Oncol 2015;26:950-8. [Crossref] [PubMed]
- Cheung WY, Renfro LA, Kerr D, et al. Determinants of Early Mortality Among 37,568 Patients With Colon Cancer Who Participated in 25 Clinical Trials From the Adjuvant Colon Cancer Endpoints Database. J Clin Oncol 2016;34:1182-9. [Crossref] [PubMed]
- Shah MA, Renfro LA, Allegra CJ, et al. Impact of Patient Factors on Recurrence Risk and Time Dependency of Oxaliplatin Benefit in Patients With Colon Cancer: Analysis From Modern-Era Adjuvant Studies in the Adjuvant Colon Cancer End Points (ACCENT) Database. J Clin Oncol 2016;34:843-53. [Crossref] [PubMed]
- Chapman JW, O'Callaghan CJ, Hu N, et al. Innovative estimation of survival using log-normal survival modelling on ACCENT database. Br J Cancer 2013;108:784-90. [Crossref] [PubMed]
- Shi Q, Renfro LA, Bot BM, et al. Comparative assessment of trial-level surrogacy measures for candidate time-to-event surrogate endpoints in clinical trials. Comp Stat Data Anal 2011;55:2748-57. [Crossref]
- Renfro LA, Shi Q, Sargent DJ, et al. Bayesian adjusted R2 for the meta-analytic evaluation of surrogate time-to-event endpoints in clinical trials. Stat Med 2012;31:743-61. [Crossref] [PubMed]
- Renfro LA, Shang H, Sargent DJ. Impact of Copula Directional Specification on Multi-Trial Evaluation of Surrogate End Points. J Biopharm Stat 2015;25:857-77. [Crossref] [PubMed]
- Renfro LA, Shi Q, Xue Y, et al. Center-Within-Trial Versus Trial-Level Evaluation of Surrogate Endpoints. Comput Stat Data Anal 2014;78:1-20. [Crossref] [PubMed]
- Renfro LA, Carlin BP, Sargent DJ. Bayesian adaptive trial design for a newly validated surrogate endpoint. Biometrics 2012;68:258-67. [Crossref] [PubMed]
- de Gramont A, Van Cutsem E, Schmoll HJ, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012;13:1225-33. [Crossref] [PubMed]
- Taieb J, Tabernero J, Mini E, et al. Oxaliplatin, fluorouracil, and leucovorin with or without cetuximab in patients with resected stage III colon cancer (PETACC-8): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:862-73. [Crossref] [PubMed]
- Midgley RS, Love S, Tomlinson I, et al. Final results from QUASAR2, a multicenter, international randomized phase III trial of capecitabine +/- bevacizumab in the adjuvant setting of stage II/III colorectal cancer. Ann Oncol 2014;25:LBA12.
- Midgley RS, McConkey CC, Johnstone EC, et al. Phase III randomized trial assessing rofecoxib in the adjuvant setting of colorectal cancer: final results of the VICTOR trial. J Clin Oncol 2010;28:4575-80. [Crossref] [PubMed]
- Weiser MR, Gönen M, Chou JF, et al. Predicting survival after curative colectomy for cancer: individualizing colon cancer staging. J Clin Oncol 2011;29:4796-802. [Crossref] [PubMed]



