
Update on skin directed therapies in mycosis fungoides
Introduction
Primary cutaneous T-cell lymphoma (CTCL) encompasses a heterogenous group of non-Hodgkin’s lymphoma (NHL), which are responsible for two-thirds of cutaneous lymphoma cases. Mycosis fungoides (MF) is the most common variant of CTCL, accounting for over half of all cases, and tends to be indolent in nature in the early stages, although it may progress to advanced stage disease. The incidence of MF is estimated at 5.6 per million persons, according to the Surveillance, Epidemiology and End Results (SEER) program of the United States National Cancer Institute and has remained steady since 1995 (1).
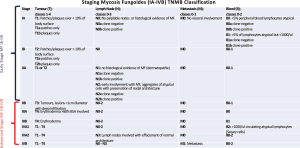
The CTCLs are currently classified according to the 2016 revision of the World Health Organization (WHO) classification of lymphoid neoplasms (2), which mostly integrates the WHO-EORTC cutaneous lymphoma classification from 2005 (3,4). The CTCL staging systems are based on the Bunn and Lamberg’s tumour, lymph node, metastasis (TNM) system established in 1979 (5), which was revised to include a blood stage, TNMB in 2007 (Figure 1) (6). There are MF variants, namely folliculotropic MF, pagetoid reticulosis, and granulomatous slack skin, which have distinct clinical presentations and prognoses (3).
MF presents with localised cutaneous patches and/or plaques in the early stages, low level nodal or blood involvement may occur. Advanced stages include skin tumours, erythroderma, and systemic involvement (extensive nodal/blood involvement or visceral involvement). Two-thirds of patients present with early stage MF (IA–IIA) with survival often of 10+ years (7) but because of the lack of any curative therapies patients suffer poor quality of life from painful, itchy and disfiguring lesions (8). A quarter of early stage patients will progress to advanced stage disease with a poor prognosis and median survival of 3 years (9). Sézary Syndrome (SS) accounts for 5% of cases, and is characterised by erythroderma, lymphadenopathy and leukemic involvement at diagnosis, with a median survival of 32 weeks (7).
Management is based on stage directed treatment with early stage MF (I1-IIA) using skin directed therapies (SDTs), including topical corticosteroids (TCS), phototherapy, topical chemotherapy or retinoids, and radiotherapy (4). There is no specific algorithm for management of early stage disease and treatments should be tailored according to individual patients needs and their side-effect profile (Table 1). Advanced stage (IIB–IV) or refractory MF often requires systemic treatments in combination with SDT for symptomatic relief. The impact of SDT in preventing MF progression is not fully known (4), and is primarily used as a palliative approach, aiming to improve the patient’s quality of life (10). SDTs may improve, pruritus, pain or clinical appearance. There is no evidence that more aggressive therapies prolong survival. The rationale is in part based on a key randomised controlled trial (RCT) comparing parenteral chemotherapy combined with electron beam radiation, against topical treatment. There were higher complete response (CR) rates in the systemic group at 38%, compared with 18% in the topical group. However, there was no significant difference in the disease-free or overall survival between the two groups after a median of 75 months follow-up. The combination group had considerable adverse effects and morbidity (11).
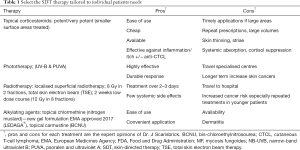
Full table
To provide standardised MF/SS trial assessments specific endpoints and response criteria were defined in a consensus statement in 2011 (12). The National Comprehensive Cancer Network Clinical Practice Guideline in Oncology on T-cell lymphomas has recently published updated guidance on the step-wise approach to MF/SS management (13). However there are only a very limited number of RCTs of SDTs in MF and most are single cohort reports. This review will focus on SDTs and their role in the management of classic MF/SS.
Topical therapies
There is limited evidence for topical therapies in MF due to the lack of RCTs or well-controlled studies. The therapies discussed have some clinical efficacy for patch and thin-plaque stage MF, however, information about specific response outcomes, such as duration of response and freedom from relapse is limited. The majority of topical therapies are not licensed for the MF usage.
Emollients
Emollients are frequently prescribed for patients with inflammatory skin conditions, including MF, and may reduce the itch sensation and scaling. Emollients reduce the transepidermal water loss, which may be further reduced with the use of humectants, that can reduce the corneocyte loss and alter the lipid barrier (10,14). A randomised, double-blind, placebo-controlled study assessed the efficacy of topical peldesine compared with emollient cream as placebo in patients with patch and plaque stage CTCL; the response rate was 28% and 24%, respectively, which was not statistically significant (15). The high emollient placebo response rate suggests the potential therapeutic value in moisturisers, which may be an important adjunctive alongside other topical therapies, and should be considered when assessing other treatments for early stage MF.
TCS
TCS are frequently prescribed for patients with early stage MF with patches or thin plaques as palliation. Despite their frequent usage, evidence for TCS is sparse. Zackheim et al. published the largest prospective study of 79 patients with stage T1 or T2 MF with the majority using class 1 TCS (very potent) mostly twice daily. Complete remission was achieved in 63% and partial remission in 31%, with a total response rate of 94% in the T1 group. The figures for the T2 patients were 25%, 57% and 82%, respectively. The response durations are rarely prolonged, and on stopping TCS therapy, only 37% of T1 and 18% of T2 patients remained in complete remission over the median follow-up period of 9 months (16). Lower strength topical steroids, fluocinolone acetonide 0.01% to 0.025%, in a small case series provided a response, which was less dramatic than stronger concentrations (17). Based on the limited data, the recommendation is to use high potency TCS over weaker concentration, which are typically well-tolerated with minimal risk of side-effects, if used in accordance with other inflammatory disease regimes (4).
Topical mechlorethamine (nitrogen mustard)
Since 1949, topical mechlorethamine (MCH, nitrogen mustard), a chemotherapeutic alkylating agent, has been approved as SDT for MF in the United States of America (USA) (4). The efficacy of MCH is around 51–84% CR for patients with stage T1 MF and 31–62.2% for T2 MF disease (18).
A key randomized, controlled, multi-centre trial with 260 patients evaluated the efficacy and safety of a novel MCH 0.02% gel compared with MCH 0.02% compounded ointment in stage IA–IIA MF. The primary endpoint was the Composite Assessment of Index Lesion Severity (CAILS), which demonstrated the MCH 0.02% gel was non-inferior to 0.02% MCH ointment with an overall RR of 58% versus 48%, respectively (19). The study was extended and 98 of the patients, who had not achieved CR applied a MCH 0.04% gel, where 26.5% achieved at least a 50% reduction of their CAILS score, 6.1% CR and 20.4% partial response, suggesting a potential benefit with the higher strength MCH, if patients fail on 0.02% (20).
These studies highlight that topical MCH is effective for early stage MF. In 2017, the European Medicines Agency (EMA) approved MCH 0.02% gel (Ledaga®) for treatment in MF. The US Food and Drug Administration approved MCH 0.016% gel (Valchlor) for stage IA and IB MF in 2013 for patients, who had received other SDTs first. This eases the treatment access as it was historically on site prepared ointment and aqueous solutions.
A French study demonstrated that twice-weekly applications with MCH 0.02% aqueous solution followed by a potent TCS for 6 months in early stage MF achieved a 58% CR rate (21). The limitation of the published MCH studies, is that they are predominantly retrospective often complicated by using other therapies alongside topical MCH. There are variable response durations to topical MCH, but stage 1A MF patients may rarely be cured. The optimal treatment regime looking at frequency, spot or whole-body applications and use of combination or maintenance therapy is yet to be established.
Local adverse effects are common, particularly irritant contact dermatitis in 10–40% of cases, but also allergic contact dermatitis and hyperpigmentation. The risk of developing secondary malignancies as a direct result of topical MCH has been controversial with conflicting results, and patients were often managed with other treatment modalities known to increase the risk, including phototherapy and total skin electron beam therapy. In 2014, a 30-year population-based cohort study comparing MF patients, who had used topical MCH with patients not having received topical MCH. They concluded there was no increased risk of non-melanoma or melanoma skin cancers or pulmonary disease or cancer. Topical MCH did not affect the mortality and cause-specific mortality, indicating it as a safe therapy (22).
Topical carmustine (BCNU)
Carmustine, also known as bis-chloroethylnitrosourea (BCNU) is an alkylating chemotherapy agent that has been used in patch and early-plaque stage MF. It needs to be compounded in an aqueous or ointment formulation. The efficacy appears similar to topical MCH with CR rates of 86%, 48% and 21% in stage T1, T2 and T4, respectively, with a median time of 11.5 weeks (23).
There are limited studies assessing the efficacy of BCNU. Compared with MCH, BCNU causes less hypersensitivity reactions, affecting around 5–10% of cases (7). The main concern with BCNU is the systemic absorption in up to 28% of patients, predisposing to myelosuppression (10). Consequently, full blood count monitoring is required and treatment given for short periods, 2–4 weeks for widespread disease. It is contraindicated to use maintenance BCNU (7).
Other topical therapies
The retinoid X-receptor bexarotene (1%) gel has been effectively used in patients where other topical therapies have failed. In a phase 1 and 2, open-label, dose-escalation trial of topical bexarotene gel the overall response rate was 63%, and CR rate of 21% in stage IA and IB disease. The response rate was higher (75%) if patients had not tried other topical therapies (67%) previously; 23 months was the estimated median response duration (24). A phase III trial assessing efficacy of topical bexarotene 1% gel in 50 patients with refractory or persistent early-stage MF patients, showed a CAILS response rate of 46% (25).
The Food and Drug Administration (FDA) has approved topical bexarotene 1% gel (Targretin®) in CTCL stage IA and IB, who have refractory or persistent disease after other treatments (26). It is currently unlicensed in Europe.
Predominantly case reports and series have suggested other topical retinoid preparations, such as tazarotene 0.1% (27,28) and alitretinoin 0.1% (29) may be helpful in early MF stages. Imiquimod 5% (30-32), 5-fluorouracil cream (33), topical methotrexate-laurocapram (34) and tacrolimus 0.1% ointment (35) may also be beneficial. It is difficult to translate the data from uncontrolled topical studies, given the high response rate with emollients alone. Future randomised controlled trials are required to validate these topical modalities efficacy in MF.
Phototherapy
Phototherapy is a frequent key therapy in managing patients with MF and tends to produce high complete remission rates with variable response duration. Broadband, narrowband UVB light and psoralen plus ultraviolet A light photochemotherapy (PUVA) are traditional treatments, but more recently UVA1 and excimer laser are other emerging modalities. UVB therapy is recommended for patch or thin plaque MF and PUVA for thicker plaques (13). In 2016, the United States Cutaneous Lymphoma Consortium published a comprehensive review of the available data and guidelines on phototherapy in MF/SS (36). Disadvantages include travel time to hospital and increase risk of other skin cancers.
Ultraviolet B (UVB) phototherapy
Broadband ultraviolet B (290–320 nm, bbUVB) is rarely in clinical use today, as it has been replaced by narrowband UVB (TL-01: 311–312 nm, nbUVB) lamps, given these are less erythemogenic and more effective in managing psoriasis (4). There are high and comparable response rates with early stage MF patients treated with bbUVB and nbUVB. A retrospective study reviewed 111 early stage MF patients treated with nbUVB and bbUVB. CR with nbUVB and bbUVB was achieved in 84% and 89% of IA patients and 78% and 44% of IB patients, respectively, after a mean time of 12.6 weeks (37).
In a review of patch and plaque stage MF patients treated nbUVB without systemic therapy, the CR rates were on average 84% (range =54% to 90%). Most received 3 treatments weekly (12/16 studies). nbUVB was more effective for patch stage MF and patients with fairer skin types (Fitzpatrick I–III). The relapse-free period ranged from 5.9 to 14.5 months in patients without maintenance nbUVB, and the relapse rate affected 29% to 100% (36).
In the literature there is a consensus that nbUVB is less effective with lower remission durations compared with PUVA, particularly for thicker plaques, but there are few comparative studies (9). A retrospective study with 95 early stage MF (IA, IB and IIA) patients treated with PUVA and 19 with nbUVB, suggested nbUVB was as effective as PUVA with compatible CR rates at 62.1% and 68.4%. There was no significant difference in the relapse times at 11.5 and 14.0 months for PUVA and nbUVB, respectively (38). In a recent case series of 34 paediatric patients with MF, 17/21 (81%) of patients treated primarily with phototherapy responded. CRs were seen in 3/18 (17%) hypopigmented MF cases, all of whom were treated with nbUVB (39).
The value of maintenance UVB therapy in MF is to be defined, but there may be a reduction in the relapse rate and prolonged relapse-free intervals in some cases (36). In stage 1A MF, which has a normal or near normal long-term survival rate, it is likely that prolonged remission has little impact on prognosis (40,41). The nbUVB data is limited by a lack of prospective RCTs.
The risk of skin cancer development with nbUVB is overall reassuring (36). A literature review of around 3,400 patients, who predominantly had psoriasis, demonstrated no overall increase in skin cancer risk if treated with UVB, but there was an increased risk with patients treated with both UVB and PUVA in one study (42). Similarly, a Scottish study reviewing nearly 3,900 patients, mostly with psoriasis, who had been treated with nbUVB, did not have a significant risk of skin cancer compared with age- and sex-matched controls. However, caution has to be applied, as the median number of nbUVB treatments was 29 with only 352 receiving ≥100 treatments (43).
PUVA photochemotherapy
UVA penetrates the dermis deeper than UVB, is more effective at treating thicker plaques or MF refractory to UVB. The British Association of Dermatologists recommends PUVA as the first-line treatment of choice for plaque stage MF (44). The NCCN recommends PUVA for early stage or advanced MF if the plaques are thicker (13). When used for MF, PUVA is often prescribed with 8-methoxypsoralen (MOP) given 2–3 times weekly. Oral 5-MOP is an alternative that is available in Europe and other parts of the world, but not in the USA, which causes less nausea (36). Bath PUVA has been shown to be effective in small case series, but is rarely used as the head is untreated, which may lead to early relapse at this site (4,45,46). Bath PUVA may be useful if systemic PUVA is not appropriate (46).
There are multiple non-randomised retrospective case series documenting the efficacy of PUVA in MF, but these are often difficult to compare, due to wide study heterogeneity. The United States Cutaneous Lymphoma Consortium summarised 6 PUVA studies and the CR rates were reported as 85%, 65%, and 85% for stage IA (130/152 patients), stage IB (114/175 patients), and stage IIA (30/35 patients), respectively (36). MF patches and thin plaques achieved CR quicker and more effectively than thicker plaques (47). A RCT showed that 25% of stage IB and IIA MF patients, who achieved CR with PUVA had a sustained duration of response (48).
There is limited data on the use of 5-MOP for MF. A retrospective study with small numbers found 5-MOP and 8-MOP PUVA to have similar efficacy in early stage MF (49).
Maintenance PUVA is an area of controversy, but is reported in the majority of studies, yet it remains uncertain if it prolongs remission (36). A small recent survey of International Society of Cutaneous Lymphoma members revealed that maintenance PUVA would be used by 88% of respondents, ranging from once weekly to once monthly (50). A single centre retrospective analysis of early stage MF evaluated long-term outcomes of patients having achieved complete remission with PUVA monotherapy. They concluded that 30–50% had prolonged remission (nearly 10 years disease-free survival rates), but the majority received maintenance PUVA. There was no difference in the overall survival rate between the relapsing and non-relapsing groups, but nearly a third of patients developed photodamage and cutaneous cancers (51). Another study by Hönigsmann et al. reported just over half (55%) of stage IA and 39% of stage IB patients treated with PUVA were disease free at the end of a mean 44 months follow-up period, but maintenance was implemented (52). Maintenance PUVA did not prevent relapses in stage IA and IB MF disease in a recent prospective study (53).
Patients with stage IIB MF, often have tumours associated with patches and plaques. Phototherapy may be helpful in achieving response in the patches and plaques, whilst the tumours are managed with for example localised radiotherapy. Erythrodermic MF/SS patients (stage III/IVA) tolerate phototherapy poorly and it may exacerbate pruritus. A review of published cases of erythrodermic MF, including some with SS, receiving PUVA monotherapy had a CR rate of 43% (16/37) (36). For advanced MF/SS, salvage PUVA therapy can be employed for persistent patches and plaques or quickly relapsing disease after systemic therapies.
High cumulative dosages of PUVA are associated with an increased risk of non-melanoma skin cancers, particularly squamous cell carcinoma (SCC) (54). A meta-analysis demonstrated that patients with psoriasis, who had been exposed to high-dose PUVA (>200 treatments or 2,000 J/cm2) had a 14 times higher incidence than low dose patients (<100 treatments or <1,000 J/cm2) of developing SCCs (55). There may also an increased incidence of melanoma, although this is controversial (36). A study found the incidence of invasive melanoma to be 10 times greater than the general population for patients having received PUVA (56). Given this increased risk of skin cancers, the British Association of Dermatologists (BAD) and British Photodermatology Group guidelines for the safe and effective use of PUVA therapy 2015 recommend limiting the lifetime cumulative exposure to 1,200 J/cm2 and/or 250 sessions (44). According to the BAD guidelines on CTCL, maintenance PUVA should ideally be avoided as it is rarely effective in preventing relapse (7). Maintenance PUVA may be considered in preventing MF that promptly relapses (44) and in rare cases of refractory MF for symptomatic benefit. This has to be carefully considered as patients with MF may require systemic chemotherapy in the future, which further increases their chances of secondary malignancy.
UVA1
UVA1 phototherapy (340–400 nm) penetrates more deeply into the dermis, compared with UVB and UVA, and small case series have shown benefit in MF (57-59). A recent case series with 19 early stage MF patients (IA–IIA) received UVA 5 times weekly for 5 weeks, and CR was 63% and partial response 37%. However, there was a high relapse rate within 3 months of stopping UVA1, affecting over half (58%) of patients who had achieved a CR (60).
UVA1 has been shown to be effective in advanced stage MF with widespread plaques, nodules and erythrodermic MF in a case series with 13 patients. CR was achieved in 85% and the remaining 15% achieved partial response, whilst the patients’ own unirradiated control lesions did not improve (57). These studies suggest UVA1 may be a useful addition to the MF treatment options but availability is limited.
Combination PUVA regimes
PUVA has been combined with systemic therapies, to try and improve efficacy and prolong remission.4 A systematic review of PUVA combination therapies concluded that for MF the addition of interferon-alpha or bexarotene was not superior to PUVA monotherapy in achieving an overall response (61). However, the combination may prolong the response and reduce the cumulative dosages of UVA, thereby reducing long-term side-effects (36). For advanced stage MF/SS, combination PUVA are not typically used as the first management step, but are employed as adjunctive or salvage therapy for residual MF lesions following other treatments for the tumours or nodal/visceral disease, although the data is lacking.
PUVA and interferon-alpha
Multiple studies have demonstrated that CR rates are often similar for PUVA combined with interferon-alpha compared to PUVA monotherapy (62-66). Retrospective trials have shown that PUVA combined with interferon-alpha reduced the cumulative dose of UVA and improved the duration of response compared with PUVA monotherapy (62,67). A prospective randomised multicentre clinic trial assessed patients with stage I and II MF, and found there was a significantly higher complete remission rate (70%) and reduced time to response in the interferon alpha 2a and PUVA group compared with interferon alpha 2a and acitretin (38% complete remission) (68).
PUVA and retinoids
Oral retinoids may reduce the chances of developing non-melanoma skin cancers (69). Hence combining retinoids with phototherapy, particularly PUVA, may be pragmatic. The Scandinavian Mycosis Fungoides Group reviewed the CR rate of retinoids plus PUVA (re-PUVA) and PUVA, which was achieved in 73% and 72% respectively, with no significant difference. However, re-PUVA led to reduced phototherapy sessions and UVA dosages. The relapse rates were similar but a few patients experienced increased remissions if maintenance retinoids were given (70). A recent study showed that low-dose bexarotene combined with PUVA in patients with relapsed or treatment-refractory MF, achieved an overall response rate of 67%, which is similar to PUVA monotherapy, and was well-tolerated (69).
Similarly, the EORTC Cutaneous Lymphoma Task Force phase III RCT comparing oral bexarotene and PUVA with PUVA alone in stage IB and IIA MF. They did not demonstrate a significant response rate or duration difference between the two groups; 71% in the PUVA group and 77% in the combination group achieved CR at a median duration of 9.7 and 5.8 months respectively. There was a non-significant trend towards fewer PUVA sessions and lower UVA dose in the combination group. Interestingly 25% of patients achieving CR with either PUVA or the combination treatment had a sustained long-term response (48). For the PUVA and retinoid studies there is often limited data regarding outcomes, such as disease-free and overall survival.
Photodynamic therapy
Photodynamic therapy (PDT) is a new treatment option in MF patients with isolated skin lesions, not responding to other SDTs, which is well-tolerated and safe. A small case series has shown PDT to be efficacy in achieving complete or partial response in 70% (7/10), and 86% (6/7) remained in remission during the 8–31 months follow-up period (71). A comparable response rate (75%) was observed in another prospective study with early stage MF (72). The role of PDT in MF management has yet to fully established.
Excimer laser
Recent evidence suggests the excimer 308 nm laser is safe and potentially effective in early stage MF. Small case series have demonstrated its efficacy on isolated patches or difficult to reach anatomical sites (73-75). Its role within MF management has not been formalized yet and availability is limited.
Radiotherapy
Localised radiotherapy
Radiotherapy is used for all stages of MF, as it is an extremely radiosensitive condition (76-78). Superficial, localised radiotherapy is often employed as a palliative measure for localised plaques and tumours, which may be performed in combination with other therapeutic modalities, including phototherapy, other SDTs or systemic therapy (4). Consensus radiotherapy guidelines have been published by the International Lymphoma Radiation Oncology Groups in 2015 (79).
Low-grade localised radiotherapy may be used successfully in stage IA–IIB MF. Neelis et al. showed a high CR rate of 92% (60 out of 65 lesions) in patients with MF treated with 8 Gy in 2 fractions, whilst the lower dose of 4 Gy in 2 fractions only achieved a response rate of 30% (80). The lowest effective radiation dose is typically used given the palliative nature. Dosages of 8–12 Gy allow repeat treatment (79) of the same or adjacent area, despite field overlap, which is particularly helpful for difficult to treat areas, such as the lower legs.
Unilesional MF is rare, but localised higher dose radiotherapy (20 to 30 Gy in 2 fractions) may have a curative role (81-84). Tumours may require higher doses (79), and the depth of the lesions can be assessed by ultrasound, CT or MRI scan as necessary. Local radiotherapy also has a role in stage III–IVA erythrodermic MF/SS if it is associated are isolated tumours or severe hand and foot involvement. For advanced MF/SS limited peripheral nodes or visceral metastases can be managed with local external beam radiotherapy (85). Protocols are based on NHL management with low radiation doses used (86).
The dose and fractionation should consider the site, lesion type, potential acute and late complications to surrounding skin and organs, and whether total skin electron beam therapy is required. If large affected areas, such as the trunk, limbs or scalp require radiotherapy, smaller dose per fractions should ideally be given. Increasingly, new radiotherapy techniques including complex matched electrons, intensity-modulated radiotherapy (IMRT) (87), helical Hi-ART therapy (88) and high-dose rate brachytherapy (89), are used to treat these areas. Curved skin surfaces, including the scalp and face can be effectively treated with these methods, providing prolonged control of MF.
Total skin electron beam radiotherapy (TSEBT)
TSEBT can be used for MF patients with extensive patches and plaques at any stage. Multiple retrospective studies have demonstrated that TSEBT has one of the highest overall response rates (90). The European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group has published guidance on clinical indications and technical delivery of TSEBT in MF management (91).
A retrospective cohort study demonstrated that stage 1A patients treated with TSEBT achieved a complete higher response rate at 97%, while it was 68% for topical MCH. The TSEBT group had a higher freedom from relapse at 59% compared with 45% for topical MCH (P<0.05), but the long-term survival was similar (41). TSEBT has also been effective in generalised patch or plaque (T2) and tumour (T3) MF, as demonstrated by a CR in stage T2 at 75% and T3 at 47%. The group also compared TSEBT monotherapy with TSEBT using topical MCH, and both treatments achieved similar freedom from relapse, progression-free survival and overall survival (92). Hence TSEBT should be considered after patients have not responded to other first or second line treatments (7,93). For more advanced MF (T4) or SS, TSEBT can be used and combined with systemic therapies (90). Jones et al. showed that 60% of erythrodermic patients (T4) receiving TSEBT had a CR and at 5 years, 26% were disease free (94).
Standard TSEBT courses induce high remission rates, and typically 30–36 Gy are given over 8–10 weeks (4). TSEBT tends be to be given once only, but repeated treatments often at lower dosages without severe toxicities are an option (85). A pooled analysis of three phase-II clinical trials using low-dose TSEBT, included 33 patients with stage IB to IIIA, had an overall response rate of 88% with a median response duration of 70.7 weeks, and repeated courses caused only mild toxicities (95). A recent prospective study assessed the efficacy of low-dose TSEBT, using 12 Gy in 8 fractions over 2 weeks in 103 patients with MF stage IB to IV. CR was observed in 18%, and 69% had a partial response with 11.8 months median response duration (96). There is a recent trend towards lower dose TSEBT (12 Gy in 8 fractions). This dose appears efficacious and may be given safely with less side-effects and repeated if needed. TSEBT using combination therapies and maintenance regimes, may improve the length of disease remission, but requires further long-term data (90).
The TSEBT beams are limited to a particular skin depth, thus reducing systemic toxicity. Acute adverse effects are dose-dependent and include local skin reactions, pain, loss of nails, and anhidrosis. Long-term effects include telangiectasias, alopecia, and secondary cutaneous cancers have been reported in patients having received multiple TSEBTs (85,97).
Conclusions
MF is a rare condition, leading to a paucity of RCTs comparing the different skin directed treatments. Treatments should be selected on an individual patient basis according to the common side-effects and preference of patients. Early stage MF patients may be controlled for many years with SDTs and periods of expectant (i.e., no therapy) are common. There are no curative therapies for early stage MF and as such patients suffer pain, itching and disfigurement for many years impacting on their quality of life (8). In addition to early stage skin lesions, skin tumours of MF are highly radiosensitive, and localised tumours may be treated with radiotherapy. The recent EMA approval of chlormethine gel will increase the availability of topical chemotherapy treatment and will be a useful addition to early stage treatments. Further studies are required to assess the efficacy of SDT combinations and maintenance therapies.
Acknowledgements
None.
Footnote
Conflicts of Interest: JJ Scarisbrick has undertaken consultancy work in the past 5 years from Takeda, Helsinn, Actelion, Malinckcrodt, Kyowa Kirin, 4SC. ML Lovgren has no conflicts of interest to declare.
References
- Korgavkar K, Xiong M, Weinstock M. Changing incidence trends of cutaneous T-cell lymphoma. JAMA Dermatol 2013;149:1295-9. [Crossref] [PubMed]
- Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016;127:2375-90. [Crossref] [PubMed]
- Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85. [Crossref] [PubMed]
- Trautinger F, Eder J, Assaf C, et al. European Organisation for Research and Treatment of Cancer consensus recommendations for the treatment of mycosis fungoides/Sézary syndrome - Update 2017. Eur J Cancer 2017;77:57-74. [Crossref] [PubMed]
- Bunn PA, Lamberg SI. Report of the Committee on Staging and Classification of Cutaneous T-Cell Lymphomas. Cancer Treat Rep 1979;63:725-8. [PubMed]
- Olsen E, Vonderheid E, Pimpinelli N, et al. Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC). Blood 2007;110:1713-22. [Crossref] [PubMed]
- Whittaker SJ, Marsden JR, Spittle M, et al. Joint British Association of Dermatologists and U.K. Cutaneous Lymphoma Group guidelines for the management of primary cutaneous T-cell lymphomas. Br J Dermatol 2003;149:1095-107. [Crossref] [PubMed]
- Wright A, Wijeratne A, Hung T, et al. Prevalence and severity of pruritus and quality of life in patients with cutaneous T-cell lymphoma. J Pain Symptom Manage 2013;45:114-9. [Crossref] [PubMed]
- Whittaker S, Hoppe R, Prince HM. How I treat mycosis fungoides and Sézary syndrome. Blood 2016;127:3142-53. [Crossref] [PubMed]
- Nguyen CV, Bohjanen KA. Skin-Directed Therapies in Cutaneous T-Cell Lymphoma. Dermatol Clin 2015;33:683-96. [Crossref] [PubMed]
- Kaye FJ, Bunn PA, Steinberg SM, et al. A randomized trial comparing combination electron-beam radiation and chemotherapy with topical therapy in the initial treatment of mycosis fungoides. N Engl J Med 1989;321:1784-90. [Crossref] [PubMed]
- Olsen EA, Whittaker S, Kim YH, et al. Clinical end points and response criteria in mycosis fungoides and Sézary syndrome: a consensus statement of the International Society for Cutaneous Lymphomas, the United States Cutaneous Lymphoma Consortium, and the Cutaneous Lymphoma Task Force of the European Organisation for Research and Treatment of Cancer. J Clin Oncol 2011;29:2598-2607. [Crossref] [PubMed]
- Horwitz SM, Ansell SM, Ai WZ. National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology T-Cell Lymphomas. J Natl Compr Canc Netw 2018;16:123-35. [Crossref] [PubMed]
- Rawlings A, Harding C, Watkinson A, et al. The effect of glycerol and humidity on desmosome degradation in stratum corneum. Arch Dermatol Res 1995;287:457-64. [Crossref] [PubMed]
- Duvic M, Olsen EA, Omura GA, et al. A phase III, randomized, double-blind, placebo-controlled study of peldesine (BCX-34) cream as topical therapy for cutaneous T-cell lymphoma. J Am Acad Dermatol 2001;44:940-7. [Crossref] [PubMed]
- Zackheim HS, Kashani-Sabet M, Amin S. Topical corticosteroids for mycosis fungoides. Experience in 79 patients. Arch Dermatol 1998;134:949-54. [Crossref] [PubMed]
- Farber EM, Cox AJ, Steinberg J, et al. Therapy of mycosis fungoides with topically applied fluocinolone acetonide under occlusive dressing. Cancer 1966;19:237-45. [Crossref] [PubMed]
- Liner K, Brown C, McGirt LY. Clinical potential of mechlorethamine gel for the topical treatment of mycosis fungoides-type cutaneous T-cell lymphoma: a review on current efficacy and safety data. Drug Des Devel Ther 2018;12:241-54. [Crossref] [PubMed]
- Lessin SR, Duvic M, Guitart J, et al. Topical chemotherapy in cutaneous T-cell lymphoma: positive results of a randomized, controlled, multicenter trial testing the efficacy and safety of a novel mechlorethamine, 0.02%, gel in mycosis fungoides. JAMA Dermatol 2013;149:25-32. [Crossref] [PubMed]
- Kim YH, Duvic M, Guitart J, et al. Efficacy and safety of mechlorethamine (MCH) 0.04% gel in mycosis fungoides (MF) after treatment with topical MCH 0.02%. J Clin Oncol 2014;32:abstr 9093.
- de Quatrebarbes J, Estève E, Bagot M, et al. Treatment of early-stage mycosis fungoides with twice-weekly applications of mechlorethamine and topical corticosteroids: a prospective study. Arch Dermatol 2005;141:1117-20. [Crossref] [PubMed]
- Lindahl LM, Fenger-Grøn M, Iversen L. Secondary cancers, comorbidities and mortality associated with nitrogen mustard therapy in patients with mycosis fungoides: a 30-year population-based cohort study. Br J Dermatol 2014;170:699-704. [Crossref] [PubMed]
- Zackheim HS, Epstein EH, Crain WR. Topical carmustine (BCNU) for cutaneous T cell lymphoma: a 15-year experience in 143 patients. J Am Acad Dermatol 1990;22:802-10. [Crossref] [PubMed]
- Breneman D, Duvic M, Kuzel T, et al. Phase 1 and 2 trial of bexarotene gel for skin-directed treatment of patients with cutaneous T-cell lymphoma. Arch Dermatol 2002;138:325-32. [Crossref] [PubMed]
- Heald P, Mehlmauer M, Martin AG, et al. Topical bexarotene therapy for patients with refractory or persistent early-stage cutaneous T-cell lymphoma: results of the phase III clinical trial. J Am Acad Dermatol 2003;49:801-15. [Crossref] [PubMed]
- Drugs@FDA: FDA Approved Drug Products. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&applno=021056, Retrieved July 26 2018.
- Apisarnthanarax N, Talpur R, Ward S, et al. Tazarotene 0.1% gel for refractory mycosis fungoides lesions: an open-label pilot study. J Am Acad Dermatol 2004;50:600-7. [Crossref] [PubMed]
- Aires D, Shaath T, Fraga G, et al. Safe and efficacious use of a topical retinoid under occlusion for the treatment of mycosis fungoides. J Drugs Dermatol 2014;13:1479-80. [PubMed]
- Bassiri-Tehrani S, Ba BA, Cohen DE. Treatment of cutaneous T-cell lymphoma with alitretinoin gel. Int J Dermatol 2002;41:104-6. [Crossref] [PubMed]
- Shipman AR, Scarisbrick J. New treatment options for mycosis fungoides. Indian J Dermatol 2016;61:119. [Crossref] [PubMed]
- Coors EA, Schuler G, Von Den Driesch P. Topical imiquimod as treatment for different kinds of cutaneous lymphoma. Eur J Dermatol 2006;16:391-3. [PubMed]
- Deeths MJ, Chapman JT, Dellavalle RP, et al. Treatment of patch and plaque stage mycosis fungoides with imiquimod 5% cream. J Am Acad Dermatol 2005;52:275-80. [Crossref] [PubMed]
- Kannangara AP, Levitan D, Fleischer AB. Six patients with early-stage cutaneous T-cell lymphoma successfully treated with topical 5-fluorouracil. J Drugs Dermatol 2010;9:1017-8. [PubMed]
- Demierre M-F, Vachon L, Ho V, et al. Phase 1/2 pilot study of methotrexate-laurocapram topical gel for the treatment of patients with early-stage mycosis fungoides. Arch Dermatol 2003;139:624-8. [Crossref] [PubMed]
- Rallis E, Economidi A, Verros C, et al. Successful treatment of patch type mycosis fungoides with tacrolimus ointment 0.1%. J Drugs Dermatol 2006;5:906-7. [PubMed]
- Olsen EA, Hodak E, Anderson T, et al. Guidelines for phototherapy of mycosis fungoides and Sézary syndrome: A consensus statement of the United States Cutaneous Lymphoma Consortium. J Am Acad Dermatol 2016;74:27-58. [Crossref] [PubMed]
- Pavlotsky F, Barzilai A, Kasem R, et al. UVB in the management of early stage mycosis fungoides. J Eur Acad Dermatol Venereol 2006;20:565-72. [Crossref] [PubMed]
- Ponte P, Serrão V, Apetato M. Efficacy of narrowband UVB vs. PUVA in patients with early-stage mycosis fungoides. J Eur Acad Dermatol Venereol 2010;24:716-21. [Crossref] [PubMed]
- Boulos S, Vaid R, Aladily TN, et al. Clinical presentation, immunopathology, and treatment of juvenile-onset mycosis fungoides: A case series of 34 patients. J Am Acad Dermatol 2014;71:1117-26. [Crossref] [PubMed]
- Zackheim HS, Amin S, Kashani-Sabet M, et al. Prognosis in cutaneous T-cell lymphoma by skin stage: long-term survival in 489 patients. J Am Acad Dermatol 1999;40:418-25. [Crossref] [PubMed]
- Kim YH, Jensen RA, Watanabe GL, et al. Clinical stage IA (limited patch and plaque) mycosis fungoides. A long-term outcome analysis. Arch Dermatol 1996;132:1309-13. [Crossref] [PubMed]
- Lee E, Koo J, Berger T. UVB phototherapy and skin cancer risk: a review of the literature. Int J Dermatol 2005;44:355-60. [Crossref] [PubMed]
- Hearn RMR, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol 2008;159:931-5. [Crossref] [PubMed]
- Ling TC, Clayton TH, Crawley J, et al. British Association of Dermatologists and British Photodermatology Group guidelines for the safe and effective use of psoralen-ultraviolet A therapy 2015. Br J Dermatol 2016;174:24-55. [Crossref] [PubMed]
- Weber F, Schmuth M, Sepp N, et al. Bath-water PUVA therapy with 8-methoxypsoralen in mycosis fungoides. Acta Derm Venereol 2005;85:329-32. [Crossref] [PubMed]
- Pavlotsky F, Hodak E, Ben Amitay D, et al. Role of bath psoralen plus ultraviolet A in early-stage mycosis fungoides. J Am Acad Dermatol 2014;71:536-41. [Crossref] [PubMed]
- Briffa DV, Warin AP, Harrington CI, et al. Photochemotherapy in mycosis fungoides. A study of 73 patients. Lancet 1980;2:49-53. [Crossref] [PubMed]
- Whittaker S, Ortiz P, Dummer R, et al. Efficacy and safety of bexarotene combined with psoralen-ultraviolet A (PUVA) compared with PUVA treatment alone in stage IB-IIA mycosis fungoides: final results from the EORTC Cutaneous Lymphoma Task Force phase III randomized clinical trial (NCT00056056). Br J Dermatol 2012;167:678-87. [Crossref] [PubMed]
- Wackernagel A, Hofer A, Legat F, et al. Efficacy of 8-methoxypsoralen vs. 5-methoxypsoralen plus ultraviolet A therapy in patients with mycosis fungoides. Br J Dermatol 2006;154:519-23. [Crossref] [PubMed]
- Carter J, Zug KA. Phototherapy for cutaneous T-cell lymphoma: online survey and literature review. J Am Acad Dermatol 2009;60:39-50. [Crossref] [PubMed]
- Querfeld C, Rosen ST, Kuzel TM, et al. Long-term follow-up of patients with early-stage cutaneous T-cell lymphoma who achieved complete remission with psoralen plus UV-A monotherapy. Arch Dermatol 2005;141:305-11. [Crossref] [PubMed]
- Hönigsmann H, Brenner W, Rauschmeier W, et al. Photochemotherapy for cutaneous T cell lymphoma: A follow-up study. J Am Acad Dermatol 1984;10:238-45. [Crossref] [PubMed]
- Sánchez MA, González T, Gaitán MF, et al. Is PUVA maintenance therapy necessary in patients with early-stage mycosis fungoides? Evaluation of a treatment guideline over a 28-month follow-up. Int J Dermatol 2011;50:1086-93. [Crossref] [PubMed]
- Nijsten TEC, Stern RS. The Increased Risk of Skin Cancer Is Persistent After Discontinuation of Psoralen+Ultraviolet A: A Cohort Study. J Invest Dermatol 2003;121:252-8. [Crossref] [PubMed]
- Stern RS, Lunder EJ. Risk of squamous cell carcinoma and methoxsalen (psoralen) and UV-A radiation (PUVA). A meta-analysis. Arch Dermatol 1998;134:1582-5. [Crossref] [PubMed]
- Stern RS. PUVA Follow up Study. The risk of melanoma in association with long-term exposure to PUVA. J Am Acad Dermatol 2001;44:755-61. [Crossref] [PubMed]
- Zane C, Leali C, Airò P, et al. “High-dose” UVA1 therapy of widespread plaque-type, nodular, and erythrodermic mycosis fungoides. J Am Acad Dermatol 2001;44:629-33. [Crossref] [PubMed]
- Aydogan K, Yazici S, Balaban Adim S, et al. Efficacy of low-dose ultraviolet a-1 phototherapy for parapsoriasis/early-stage mycosis fungoides. Photochem Photobiol 2014;90:873-7. [PubMed]
- Jang MS, Kang DY, Jeon YS, et al. Ultraviolet A1 Phototherapy of Mycosis Fungoides. Ann Dermatol 2013;25:104-7. [Crossref] [PubMed]
- Adışen E, Tektaş V, Erduran F, et al. Ultraviolet A1 Phototherapy in the Treatment of Early Mycosis Fungoides. Dermatology 2017;233:192-8. [Crossref] [PubMed]
- Humme D, Nast A, Erdmann R, et al. Systematic review of combination therapies for mycosis fungoides. Cancer Treat Rev 2014;40:927-33. [Crossref] [PubMed]
- Kuzel TM, Roenigk HH, Samuelson E, et al. Effectiveness of interferon alfa-2a combined with phototherapy for mycosis fungoides and the Sézary syndrome. J Clin Oncol 1995;13:257-63. [Crossref] [PubMed]
- Chiarion-Sileni V, Bononi A, Fornasa CV, et al. Phase II trial of interferon-alpha-2a plus psolaren with ultraviolet light A in patients with cutaneous T-cell lymphoma. Cancer 2002;95:569-75. [Crossref] [PubMed]
- Rupoli S, Barulli S, Guiducci B, et al. Low dose interferon-alpha2b combined with PUVA is an effective treatment of early stage mycosis fungoides: results of a multicenter study. Cutaneous-T Cell Lymphoma Multicenter Study Group. Haematologica 1999;84:809-13. [PubMed]
- Nikolaou V, Siakantaris MP, Vassilakopoulos TP, et al. PUVA plus interferon α2b in the treatment of advanced or refractory to PUVA early stage mycosis fungoides: a case series. J Eur Acad Dermatol Venereol 2011;25:354-7. [Crossref] [PubMed]
- Wozniak MB, Tracey L, Ortiz-Romero PL, et al. Psoralen plus ultraviolet A +/- interferon-alpha treatment resistance in mycosis fungoides: the role of tumour microenvironment, nuclear transcription factor-kappaB and T-cell receptor pathways. Br J Dermatol 2009;160:92-102. [Crossref] [PubMed]
- Hüsken AC, Tsianakas A, Hensen P, et al. Comparison of pegylated interferon α-2b plus psoralen PUVA versus standard interferon α-2a plus PUVA in patients with cutaneous T-cell lymphoma. J Eur Acad Dermatol Venereol 2012;26:71-8. [Crossref] [PubMed]
- Stadler R, Otte HG, Luger T, et al. Prospective randomized multicenter clinical trial on the use of interferon -2a plus acitretin versus interferon -2a plus PUVA in patients with cutaneous T-cell lymphoma stages I and II. Blood 1998;92:3578-81. [PubMed]
- Papadavid E, Antoniou C, Nikolaou V, et al. Safety and efficacy of low-dose bexarotene and PUVA in the treatment of patients with mycosis fungoides. Am J Clin Dermatol 2008;9:169-73. [Crossref] [PubMed]
- Thomsen K, Hammar H, Molin L, et al. Retinoids plus PUVA (RePUVA) and PUVA in mycosis fungoides, plaque stage. A report from the Scandinavian Mycosis Fungoides Group. Acta Derm Venereol 1989;69:536-8. [PubMed]
- Kim ST, Kang DY, Kang JS, et al. Photodynamic therapy with methyl-aminolaevulinic acid for mycosis fungoides. Acta Derm Venereol 2012;92:264-8. [Crossref] [PubMed]
- Quéreux G, Brocard A, Saint-Jean M, et al. Photodynamic therapy with methyl-aminolevulinic acid for paucilesional mycosis fungoides: a prospective open study and review of the literature. J Am Acad Dermatol 2013;69:890-7. [Crossref] [PubMed]
- Deaver D, Cauthen A, Cohen G, et al. Excimer laser in the treatment of mycosis fungoides. J Am Acad Dermatol 2014;70:1058-60. [Crossref] [PubMed]
- Meisenheimer JL. Treatment of mycosis fungoides using a 308-nm excimer laser: two case studies. Dermatol Online J 2006;12:11. [PubMed]
- Mori M, Campolmi P, Mavilia L, et al. Monochromatic excimer light (308 nm) in patch-stage IA mycosis fungoides. J Am Acad Dermatol 2004;50:943-5. [Crossref] [PubMed]
- Cotter GW, Baglan RJ, Wasserman TH, et al. Palliative radiation treatment of cutaneous mycosis fungoides--a dose response. Int J Radiat Oncol Biol Phys 1983;9:1477-80. [Crossref] [PubMed]
- Kirova YM, Piedbois Y, Haddad E, et al. Radiotherapy in the management of mycosis fungoides: indications, results, prognosis. Twenty years experience. Radiother Oncol 1999;51:147-51. [Crossref] [PubMed]
- Hoppe RT, Abel EA, Deneau DG, et al. Mycosis fungoides: management with topical nitrogen mustard. J Clin Oncol 1987;5:1796-803. [Crossref] [PubMed]
- Specht L, Dabaja B, Illidge T, et al. Modern radiation therapy for primary cutaneous lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 2015;92:32-9. [Crossref] [PubMed]
- Neelis KJ, Schimmel EC, Vermeer MH, et al. Low-dose palliative radiotherapy for cutaneous B- and T-cell lymphomas. Int J Radiat Oncol Biol Phys 2009;74:154-8. [Crossref] [PubMed]
- Ally MS, Pawade J, Tanaka M, et al. Solitary mycosis fungoides: a distinct clinicopathologic entity with a good prognosis: a series of 15 cases and literature review. J Am Acad Dermatol 2012;67:736-44. [Crossref] [PubMed]
- Piccinno R, Caccialanza M, Çuka E, et al. Localized conventional radiotherapy in the treatment of Mycosis Fungoides: our experience in 100 patients. J Eur Acad Dermatol Venereol 2014;28:1040-4. [Crossref] [PubMed]
- Micaily B, Miyamoto C, Kantor G, et al. Radiotherapy for unilesional mycosis fungoides. Int J Radiat Oncol Biol Phys 1998;42:361-4. [Crossref] [PubMed]
- Wilson LD, Kacinski BM, Jones GW. Local superficial radiotherapy in the management of minimal stage IA cutaneous T-cell lymphoma (Mycosis Fungoides). Int J Radiat Oncol Biol Phys 1998;40:109-15. [Crossref] [PubMed]
- Tandberg DJ, Craciunescu O, Kelsey CR. Radiation Therapy for Cutaneous T-Cell Lymphomas. Dermatol Clin 2015;33:703-13. [Crossref] [PubMed]
- Sawyer EJ, Timothy AR. Low dose palliative radiotherapy in low grade non-Hodgkin’s lymphoma. Radiother Oncol 1997;42:49-51. [Crossref] [PubMed]
- Ostheimer C, Janich M, Hübsch P, et al. The treatment of extensive scalp lesions using coplanar and non-coplanar photon IMRT: a single institution experience. Radiat Oncol 2014;9:82. [Crossref] [PubMed]
- Schaff EM, Rosenberg SA, Olson SJ, et al. Bone marrow suppression as a complication of total skin helical tomotherapy in the treatment of mycosis fungoides. Radiat Oncol 2018;13:67. [Crossref] [PubMed]
- DeSimone JA, Guenova E, Carter JB, et al. Low-dose high-dose-rate brachytherapy in the treatment of facial lesions of cutaneous T-cell lymphoma. J Am Acad Dermatol 2013;69:61-5. [Crossref] [PubMed]
- Elsayad K, Susek KH, Eich HT. Total Skin Electron Beam Therapy as Part of Multimodal Treatment Strategies for Primary Cutaneous T-Cell Lymphoma. Oncol Res Treat 2017;40:244-252. [Crossref] [PubMed]
- Jones GW, Kacinski BM, Wilson LD, et al. Total skin electron radiation in the management of mycosis fungoides: Consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol 2002;47:364-70. [Crossref] [PubMed]
- Navi D, Riaz N, Levin YS, et al. The Stanford University experience with conventional-dose, total skin electron-beam therapy in the treatment of generalized patch or plaque (T2) and tumor (T3) mycosis fungoides. Arch Dermatol 2011;147:561-7. [Crossref] [PubMed]
- Hamminga B, Noordijk EM, Vloten WA, van . Treatment of Mycosis Fungoides: Total-Skin Electron-Beam Irradiation vs Topical Mechlorethamine Therapy. Arch Dermatol 1982;118:150-3. [Crossref] [PubMed]
- Jones GW, Rosenthal D, Wilson LD. Total skin electron radiation for patients with erythrodermic cutaneous T-cell lymphoma (mycosis fungoides and the Sézary syndrome). Cancer 1999;85:1985-95. [PubMed]
- Hoppe RT, Harrison C, Tavallaee M, et al. Low-dose total skin electron beam therapy as an effective modality to reduce disease burden in patients with mycosis fungoides: results of a pooled analysis from 3 phase-II clinical trials. J Am Acad Dermatol 2015;72:286-92. [Crossref] [PubMed]
- Morris S, Scarisbrick J, Frew J, et al. The Results of Low-Dose Total Skin Electron Beam Radiation Therapy (TSEB) in Patients With Mycosis Fungoides From the UK Cutaneous Lymphoma Group. Int J Radiat Oncol Biol Phys 2017;99:627-33. [Crossref] [PubMed]
- Stein ME, Anacak Y, Zaidan J, et al. Second primary tumors in mycosis fungoides patients: experience at the Northern Israel Oncology Center (1979-2002). J BUON 2006;11:175-80. [PubMed]


