Evolution of the Chinese staging system for nasopharyngeal carcinoma
Introduction
In mainland China, the first case of nasopharyngeal carcinoma (NPC) was identified in 1930s. It was later found that NPC was mainly prevalent in five provinces of southern China including Guangdong, Guangxi, Hunan, Jiangxi, and Fujian. Radiotherapy (RT) is the primary treatment modality for NPC due to its complex anatomic location, biological behavior and high radiosensitivity. The RT of NPC in China has been used since 1940s. Decades of development, advances in external irradiation technology, RT software, and clinical experience, has improved survival rates up to 80% (1-3).
An accurate staging system holds the key to successful treatment strategies, prediction of clinical outcomes, and international communication (4). With advances in diagnostic imaging and radiation technology, as well as the biological features of NPC, the revised Chinese staging system for NPC evolved from experience to evidence-based practice.
History of Chinese staging system for NPC
Although China developed independent criteria for clinical staging of NPC since 1959, the first TNM staging system was established in Shanghai in 1965. It was based on the extent of tumor as an indicator of prognosis. Clinical experience suggests that NPC patients with large, fixed cervical lymph nodes or supraclavicular lymph node metastases had shorter survival time. The symptoms of cranial nerve palsy were often caused by lymphadenectasis. Thus, four posterior cranial nerves (IX, X, XI and XII) were also defined as N disease for several years. In 1979, it was revised into Changsha staging system in which the cranial nerves involvement was finally defined as T classification. In 1981, after reviewing the Changsha and Ho’s staging system [1978] (5), the Guangzhou staging system was established. In a major update, the tumor confined to nasopharynx was assigned T1 irrespective of the involvement of the lateral. Additionally, the size of lymph node was considered as an N classification factor (6) (Table 1).
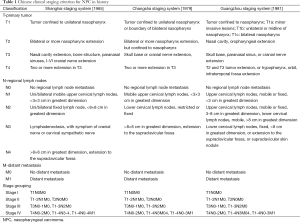
Full table
Chinese 1992 staging system based on computed tomography (CT)
The Chinese 1992 staging system was based on the retrospective data of Sun Yat-sen University reported by Min et al. (1). Four hundred and twenty-one NPC patients undergoing CT scan before primary definitive RT between 1985 and 1987 were enrolled and analyzed. All the potential prognostic factors that affect T and N classifications including physical examination, tumor involvement in CT scan and host factors at the time of the patient presentation were included in the multivariate analysis with Cox proportional hazards. The minor and major stratification risk factors were obtained to develop the new staging criteria. The implementation of this staging system established a precedent for evidence-based clinical staging system in China, and actively promoted the study of NPC.
In early 1990s, the two-dimensional conventional RT with two to three facial fields combined with an anterior-posterior whole neck field resulted in a 5-year overall survival of about 50% (1,7). Subsequently, the two bilateral facio-cervical fields were wildly accepted and resulted in a higher 5-year overall survival of 60–70% (8,9). Intensity modulated radiation therapy (IMRT) (9), chemoradiotherapy (10), and magnetic resonance imaging (MRI)-based irradiation (11) were now used across China resulting in an increased 5-year survival rate of 80%.
The limitations of the Chinese staging system [1992] were mainly two-fold: firstly, it was based on CT criteria. However, compared with CT, MRI altered the clinical stage in more than 30% of patients (11). Secondly, anatomical structures such as temporal fossa, retropharyngeal lymph nodes (RLN), cranial nerves, nasal cavity, and parapharyngeal space were not clearly defined. In addition, the N criteria primarily measured during clinical examination, were highly unreliable and dependent on physicians’ experience (12).
Therefore, the Chinese staging system of 1992 no longer represented the ideal criteria under the new circumstances. Should we just discard it and switch to the commonly used American Joint Committee on Cancer (AJCC) staging system? Following extensive discussion, the consensus in mainland China was that both the staging systems were imperfect, and additional clinical studies were needed to establish a more acceptable staging system, especially at cancer centers of Southern China, which has the highest incidence rates of NPC in the world. It was of utmost importance given that more than 95% of the newly diagnosed NPC patients in China were Epstein-Barr virus (EBV) positive for undifferentiated nonkeratinizing carcinoma (WHO III histology type).
Chinese 2008 staging system based on MRI
With the aim of building a platform for the study of the Chinese staging system and guaranteeing the continuity of the investigation into NPC, the Chinese Committee for Staging of Nasopharyngeal Carcinoma (CCSNPC) was founded in Guangzhou, China, in December 2008. After extensive evaluation and discussion, a preliminary revision of the Chinese 1992 staging system resulted in drafting the Chinese 2008 staging system for NPC, which was a consensus based on a comprehensive literature review. Changes in the staging system are as follows (Table 2) (12):
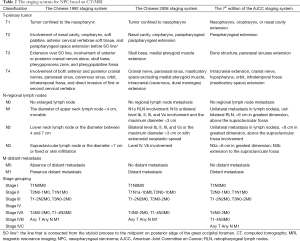
Full table
- Parapharyngeal involvement including pre-styloid space and post-styloid space were staged as T2;
- Any cranial nerve involvement was considered as T4;
- T classification was simplified; structures, such as anterior cervical vertebrae soft tissue, soft palatine, pterygopalatine fossa, orbit, and cervical vertebrae, were eliminated;
- The definition of masticator space was used in place of infratemporal fossa;
- RLN involvement was classified as N1a, either unilateral or bilateral;
- N classification was based on MRI and judged according to the criteria of the Radiation Therapy Oncology Group (RTOG), and the traditional nomenclature was no longer needed. In addition, the site, size, laterality, and extranodal neoplastic spread were enrolled in the criteria of the N category.
Further, the revised staging defined each anatomical structure including parapharyngeal space involvement described as tumor invasion across buccopharyngeal fascia, the boundary between the nasopharyngeal and the nasal cavity as the posterior of the maxillary sinus, which improved the interpretation and reduced subjective bias.
Most significantly, the new staging system considered MRI as the preferred imaging modality for NPC staging. The MRI criteria and report template were established. The diagnostic criteria of cervical lymph node metastasis based on imaging modality were stated as follows.
- A minimum diameter of not less than 10 mm on cross-sectional images;
- Central necrosis or rim enhancement;
- More than three lymph nodes in a high-risk region, and at least one of the involved lymph nodes with the minimum diameter on the largest cross-sectional images not less than 8 mm. The high-risk region was described as follows: level II for N0, followed by the next level of lymph node involvement for N-positive patients;
- Extranodal neoplastic spread, such as irregular enhancement at the edge of the lymph node, with partially or completely disappearing fat space, and lymph node convergence;
- RLN: minimum diameter on the largest cross-sectional images not less than 5 mm.
These criteria of lymph node measurement on MRI images redefined the lymph node clusters and extranodal neoplastic spread, and reduced the subjectivity of clinical diagnosis.
Chinese 2008 staging system vs. 7th edition AJCC staging system
The 6th edition AJCC staging system was commonly used in the rest of the world when the Chinese 2008 staging system was revised (13). The anatomical structures such as RLN and infratemporal fossa were poorly defined in the Chinese 1992 staging system similar to the 6th AJCC staging system. In 2010, the AJCC committee published the revised 7th edition of the staging system (14). Compared with the previous edition, the changes were as follows (Table 2):
- Oropharynx and nasal cavity involvement was assigned T1 instead of T2a;
- Parapharyngeal space involvement was classified as T2 disease;
- RLN was categorized as N1 subgroup.
Compared with the Chinese staging system [2008], the controversies related to:
- Whether or not masticator space involvement including the medial and lateral pterygoid muscles should be classified as T4 (15,16);
- Whether or not the extranodal neoplastic spread based on MRI should be included under N classification (17).
A retrospective study of a large number of cases showed that the prognostic value of the T classification of the AJCC system was better, whereas the N classification of the Chinese 2008 was superior (18,19). However, the measurement of extranodal cervical lymph node on MRI was still controversial (20). The CCSNPC conducted a prospective multicenter study to evaluate the two staging systems of NPC, in 1,508 cases at nine different cancer centers in mainland China. A preliminary report revealed that the distribution of cases, the prognosis of clinical staging and T classification of the two staging systems were similar, while the prognostic value of N classification of the Chinese 2008 was superior. However, additional evidence was still needed (21).
Future development of staging system
The revisions in the Chinese 2008 staging system and the 7th edition of the AJCC staging system, were based on retrospective analysis of NPC patients who were treated with conventional RT. Currently, IMRT is regarded as the standard treatment modality for NPC. Local control rates improved around 10% with IMRT when compared with conventional RT (22,23), which was a huge challenge for the current staging system (24). Prospective multicenter studies may avoid the defects of the retrospective analysis and provide more accurate estimates of staging system supported by robust evidence for staging revisions.
The expression of virus EB-DNA was used to evaluate the treatment outcomes in recent studies. Leung et al. found that the EB-DNA had an independent prognostic value and suggested its role as a biological factor in the NPC staging system (25). However, there were significant differences in the EBV DNA expression levels detected in different studies. The cut-off value was a major issue for inclusion of EBV DNA in the current staging system (26).
A few studies indicated that the primary gross tumor volume (GTV) had a prognostic value and therefore, should be incorporated into the current staging system (27-29). However, the measurement of GTV was not based on consensus, currently. Further studies should be initiated to confirm its positive effect on staging system (30).
Recent studies found that certain biomarkers with potential prognostic value included miRNAs (31), EBV miRNAs (32), lactotransferrin (33), LDH (34), hemoglobin, and neutrophil-to-lymphocyte ratio and platelets (35). Additional studies are needed to establish the role of these molecular biomarkers before incorporating them into the clinical staging system.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Min H, Hong M, Ma J, et al. A new staging system for nasopharyngeal carcinoma in China. Int J Radiat Oncol Biol Phys 1994;30:1037-42. [Crossref] [PubMed]
- Liu MZ, Tang LL, Zong JF, et al. Evaluation of sixth edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement. Int J Radiat Oncol Biol Phys 2008;70:1115-23.
- Lin S, Pan J, Han L, et al. Update report of nasopharyngeal carcinoma treated with reduced-volume intensity-modulated radiation therapy and hypothesis of the optimal margin. Radiother Oncol 2014;110:385-9. [Crossref] [PubMed]
- Gospodarowicz MK, Miller D, Groome PA, et al. The process for continuous improvement of the TNM classification. Cancer 2004;100:1-5. [Crossref] [PubMed]
- Ho JH. Stage classification of nasopharyngeal carcinoma: a review. IARC Sci Publ 1978.99-113. [PubMed]
- Xia YF. Practical radiotherapy for nasopharyngeal carcinoma. Beijing: Peking University Medical Press, 2003:77-83. In Chinese.
- Wu S, Zhao C, Lu T, et al. Influence of prolonged overall treatment time and interruptions on outcome in continuous radiotherapy for nasopharyngeal carcinoma. Chin J Cancer 2000;19:923-26.
- Lu T, Luo W, Zhao C, et al. A probe of design methods of block shielding facio-cervical portals at isocentre for radiotherapy of nasopharyngeal carcinoma. Chin J Cancer 2000;19:930-3.
- Lu TX, Mai WY, Teh BS, et al. Initial experience using intensity-modulated radiotherapy for recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2004;58:682-7. [Crossref] [PubMed]
- Ma J, Mai HQ, Hong MH, et al. Results of a prospective randomized trial comparing neoadjuvant chemotherapy plus radiotherapy with radiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma. J Clin Oncol 2001;19:1350-7. [PubMed]
- Liao XB, Mao YP, Liu LZ, et al. How does magnetic resonance imaging influence staging according to AJCC staging system for nasopharyngeal carcinoma compared with computed tomography? Int J Radiat Oncol Biol Phys 2008;72:1368-77. [Crossref] [PubMed]
- Chinese Committee for Staging of Nasopharyngeal Carcinoma. Report on revision of the Chinese 1992 staging system for nasopharyngeal carcinoma. Chin J Radiat Oncol 2009;18:2-6. In Chinese.
- Frederick LG, David LP, Irvin DF, et al. AJCC cancer staging handbook from the AJCC cancer staging manual. Sixth Edition. New York: Springer, 2002.
- Edge SB, Byrd DR, Compton CC, et al. AJCC Cancer Staging Manual. Seventh Edition. New York: Springer, 2009.
- Xiao Y, Pan J, Chen Y, et al. Prognostic value of MRI-derived masticator space involvement in IMRT-treated nasopharyngeal carcinoma patients. Radiat Oncol 2015;10:204. [Crossref] [PubMed]
- Sze H, Chan LL, Ng WT, et al. Should all nasopharyngeal carcinoma with masticator space involvement be staged as T4? Oral Oncol 2014;50:1188-95. [Crossref] [PubMed]
- Guo Q, Pan J, Zong J, et al. Suggestions for lymph node classification of UICC/AJCC staging system: a retrospective study based on 1197 nasopharyngeal carcinoma patients treated with intensity-modulated radiation therapy. Medicine (Baltimore) 2015;94:e808. [Crossref] [PubMed]
- Pan J, Xu Y, Qiu S, et al. A comparison between the Chinese 2008 and the 7th edition AJCC staging systems for nasopharyngeal carcinoma. Am J Clin Oncol 2015;38:189-96.
- OuYang PY, Su Z, Ma XH, et al. Comparison of TNM staging systems for nasopharyngeal carcinoma, and proposal of a new staging system. Br J Cancer 2013;109:2987-97. [Crossref] [PubMed]
- Zong J, Lin S, Lin J, et al. Impact of intensity-modulated radiotherapy on nasopharyngeal carcinoma: Validation of the 7th edition AJCC staging system. Oral Oncol 2015;51:254-9.
- Lin S, Chen X, He X, et al. Preliminary results of a prospective multicenter study on clinical staging system for nasopharyngeal carcinoma. Chin J Radiat Oncol 2015;24:275-80.
- Qu S, Liang ZG, Zhu XD. Advances and challenges in intensity-modulated radiotherapy for nasopharyngeal carcinoma. Asian Pac J Cancer Prev 2015;16:1687-92. [Crossref] [PubMed]
- Lee AW, Ng WT, Chan LL, et al. Evolution of treatment for nasopharyngeal cancer--success and setback in the intensity-modulated radiotherapy era. Radiother Oncol 2014;110:377-84. [Crossref] [PubMed]
- Ng WT, Yuen KT, Au KH, et al. Staging of nasopharyngeal carcinoma--the past, the present and the future. Oral Oncol 2014;50:549-54. [Crossref] [PubMed]
- Leung SF, Zee B, Ma BB, et al. Plasma Epstein-Barr viral deoxyribonucleic acid quantitation complements tumor-node-metastasis staging prognostication in nasopharyngeal carcinoma. J Clin Oncol 2006;24:5414-8. [Crossref] [PubMed]
- Yip TT, Ngan RK, Fong AH, et al. Application of circulating plasma/serum EBV DNA in the clinical management of nasopharyngeal carcinoma. Oral Oncol 2014;50:527-38. [Crossref] [PubMed]
- Chua DT, Sham JS, Kwong DL, et al. Volumetric analysis of tumor extent in nasopharyngeal carcinoma and correlation with treatment outcome. Int J Radiat Oncol Biol Phys 1997;39:711-9. [Crossref] [PubMed]
- Sze WM, Lee AW, Yau TK, et al. Primary tumor volume of nasopharyngeal carcinoma: prognostic significance for local control. Int J Radiat Oncol Biol Phys 2004;59:21-7. [Crossref] [PubMed]
- Guo R, Sun Y, Yu XL, et al. Is primary tumor volume still a prognostic factor in intensity modulated radiation therapy for nasopharyngeal carcinoma? Radiother Oncol 2012;104:294-9. [Crossref] [PubMed]
- Liu D, Long G, Mei Q, et al. Primary tumor volume should be included in the TNM staging system of nasopharyngeal carcinoma. Med Hypotheses 2014;82:486-7. [Crossref] [PubMed]
- Liu N, Cui RX, Sun Y, et al. A four-miRNA signature identified from genome-wide serum miRNA profiling predicts survival in patients with nasopharyngeal carcinoma. Int J Cancer 2014;134:1359-68. [Crossref] [PubMed]
- Zhang G, Zong J, Lin S, et al. Circulating Epstein-Barr virus microRNAs miR-BART7 and miR-BART13 as biomarkers for nasopharyngeal carcinoma diagnosis and treatment. Int J Cancer 2015;136:E301-12. [Crossref] [PubMed]
- Zhang W, Fan S, Zou G, et al. Lactotransferrin could be a novel independent molecular prognosticator of nasopharyngeal carcinoma. Tumour Biol 2015;36:675-83. [Crossref] [PubMed]
- Wan XB, Wei L, Li H, et al. High pretreatment serum lactate dehydrogenase level correlates with disease relapse and predicts an inferior outcome in locally advanced nasopharyngeal carcinoma. Eur J Cancer 2013;49:2356-64. [Crossref] [PubMed]
- Chang H, Gao J, Xu BQ, et al. Haemoglobin, neutrophil to lymphocyte ratio and platelet count improve prognosis prediction of the TNM staging system in nasopharyngeal carcinoma: development and validation in 3,237 patients from a single institution. Clin Oncol (R Coll Radiol) 2013;25:639-46. [Crossref] [PubMed]


