
High local control and low ocular toxicity using ultra-low-dose “boom-boom” radiotherapy for indolent orbital lymphoma
Highlight box
Key findings
• Ultra-low dose radiation (“boom-boom” RT, 4 Gy in 2 fractions) provides excellent local control with low toxicity.
What is known and what is new?
• Ophthalmologist reported higher toxicity than oncology: 33.3% new post-RT toxicities including dry eye, cataract, and chorioretinal atrophy.
What is the implication, and what should change now?
• Further prospective randomized studies are needed to better define the outcome and toxicity of ultra-low-dose (4 Gy) RT for ocular lymphoma.
Introduction
Orbital non-Hodgkin lymphomas (NHL) arise extranodally in various parts of the ocular adnexa, including the orbit, eyelid, conjunctiva, lacrimal gland, and orbital (1). They comprise 1% of all lymphomas, 8% of extranodal lymphomas, and 50–60% of ocular adnexal lymphomas with increasing incidence (1,2). The majority of orbital lymphomas are indolent types. Extranodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) is most common (3). Other types may also occur, such as follicular lymphoma, mantle lymphoma. These orbital lymphomas have an indolent clinical course with favorable prognosis. However, they may cause visual disturbance, cosmetic issue, and affect quality of life.
The first line of treatment for early-stage indolent lymphomas is irradiation (4). Conventional radiation with doses of 24–30 Gy provides high local control rates (5,6). However, the orbital structures are uniquely sensitive to radiation and may develop toxicities including dry eye, conjunctivitis, cataracts, keratoconjunctivitis sicca, and radiation retinopathy (6). Given the competing goals of local control and minimizing ocular toxicities, the ultra-low-dose (4 Gy in 2 fractions) treatment regimen, colloquially termed “boom-boom,” has been investigated (7-13). However, the efficacy of “boom-boom” regimen is still controversial, and not adopted widely. The detail of ophthalmologic toxicity after RT in orbital lymphoma reports is also limited. In this study, we report outcomes in indolent orbital lymphoma treated with the “boom-boom” regimen with an emphasis on outcome and toxicity based on ophthalmological evaluation. We present the following article in accordance with the STROBE reporting checklist (available at https://cco.amegroups.com/article/view/10.21037/cco-22-84/rc).
Methods
This retrospective case series study was approved by the Institutional Review Board of Thomas Jefferson University (IRB# 18D.480) and is in compliance with the tenets set by the Declaration of Helsinki (as revised in 2013) and the Health Insurance Portability and Accountability Act. Patient consent was granted to obtain pertinent health information.
Adult patients with indolent orbital lymphoma treated at Thomas Jefferson University Hospital with 4 Gy in 2 fractions between January 2017 and June 2022 were included. Patient clinical, pathologic, treatment, and toxicity variables as described by medical oncology, radiation oncology, and ophthalmology were recorded and analyzed. These assessments were done at least by 1 radiation oncologist (W Shi), 1 medical oncologist (P Porcu, U Martinez-Outschoorn, O Alpdogan) and 1 ophthalmologist (SE Lally, CL Shields), who are specialists with over 10 years of experience.
All patients were treated with RT of 4 Gy in 2 fractions. All patients underwent computed tomography (CT) simulation with aquaplastic mask immobilization. All patients were treated with Truebeam® (Varian, Palo Alto, CA, USA). External beam radiation with 3-dimensional (3D) planning was performed for all patients, except for patients with superficial conjunctival MALT lymphoma, who were treated with en face electron. For patients other than localized conjunctival MALT lymphoma, gross tumor volume (GTV) was delineated using CT simulation and prior diagnostic scans. Clinical target volume included the entire ipsilateral orbit and planning target volume (PTV) expansion was 0.5 cm. Image guidance included kilovoltage (kV) and megavoltage (MV) imaging. Treatment was typically delivered using 6 MV photons with 3D conformal techniques. Treating physician is a board-certified radiation oncologist subspecialized in lymphoma with over 10-year experience.
Patients underwent follow-up with medical oncologists, radiation oncologists, and ophthalmologists, where oncologists reported toxicity using Oncologist-reported Common Terminology Criteria for Adverse Events (CTCAE), version 5, grading, and ophthalmologists used in-depth ocular reports. These reports detailed not only patient-reported complaints, but also changes in best-corrected visual acuity (BCVA), intraocular pressure, grading of cataracts, and fundus examinations. Significant change in BCVA was defined as gain or loss of at least three lines on log[minimum angle of resolution (MAR)] charts.
Descriptive analysis of patient, disease, treatment, and toxicity characteristics was performed. Endpoints of interest included response rate, local control, distant progression, overall survival, and ocular toxicity as per CTCAE and ophthalmology reports. Local control was assessed using clinical and radiologic evaluation.
Results
Between January 2017 and June 2022, a total of 17 patients with 19 orbits with indolent lymphoma were treated at Thomas Jefferson University with low dose (4 Gy in 2 fractions) boom-boom regimen. The cohort consisted of 12 (71%) women and 5 (29%) men. Of the 17 patients, 14 (82%) were Caucasian, 2 (12%) were African American, and 1 (6%) was Hispanic. Median patient age was 67 years (range, 24–80 years). Karnofsky Performance Score was >70 in all patients. Presenting symptoms included decreased vision, pain, lump, ptosis, swelling, redness, and proptosis.
Histology included mucosa-associated lymphoma tissue (MALT, 5 patients), follicular lymphoma (4 patients), marginal zone lymphoma (3 patients), mantle cell lymphoma (1 patient), and other low-grade lymphomas (4 patients). For the total 17 patients with 19 involved orbits, the various affected sites in the eye included orbit (8 patients), conjunctiva (4 patients), lacrimal gland (4 patients), choroid (2 patients), and eyelid (1 patient), with 2 patients with bilateral orbits involvement. The Lugano classification for all patients were: stage I 13 patients (76%), stage II 3 patients (18%) and stage IV 1 patient (6%). Fifteen (88%) patients had unilateral ocular involvement, and 2 (12%) patients had bilateral involvement. Three (18%) patients had multi-centric orbital disease. Majority (88%) of our patients had no prior ocular history, 2 have early-stage cataract. No patient had previous radiation treatment. Table 1 provides a summary of patient and disease characteristics.
Table 1
| Patient characteristics | Values |
|---|---|
| Number of patients | 17 |
| Age in years, median [range] | 67 [24–80] |
| Sex, n [%] | 17 [100] |
| Female | 12 [71] |
| Male | 5 [29] |
| Race, n [%] | 17 [100] |
| White/Caucasian | 14 [82] |
| Black/African American | 2 [12] |
| Hispanic | 1 [6] |
| Ocular History, n [%] | 17 [100] |
| No | 15 [88] |
| Yes | 2 [12] |
| Karnofsky Performance Score, n [%] | 17 [100] |
| 80–100 | 17 [100] |
| 10–70 | 0 [0] |
| Affected orbit, n [%] | 17 [100] |
| Unilateral | 15 [88] |
| Bilateral | 2 [12] |
| Histology, n [%] | 17 [100] |
| MALT lymphoma | 5 [29] |
| Other low-grade lymphoma | 4 [24] |
| Follicular lymphoma | 4 [24] |
| Marginal zone lymphoma | 3 [18] |
| Mantle cell lymphoma | 1 [6] |
| Lugano stage, n [%] | 17 [100] |
| Stage I/II | 16 [94] |
| Stage III/IV | 1 [6] |
| Affected site, n [% orbits] | 17 patients, 19 orbits [100] |
| Orbit | 8 [42] |
| Conjunctiva | 4 [21] |
| Lacrimal gland | 4 [21] |
| Choroid | 2 [11] |
| Eyelid | 1 [5] |
| Optic nerve involvement, n [% orbits] | 19 orbits [100] |
| No | 18 [95] |
| Yes | 1 [5] |
| Previous chemotherapy, n [%] | 17 [100] |
| No | 17 [100] |
| Yes | 0 [0] |
| Previous radiotherapy, n [%] | 17 [100] |
| No | 17 [100] |
| Yes | 0 [0] |
MALT, mucosa-associated lymphoid tissue.
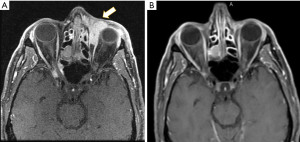
Median follow-up was 39 months (range, 11–52 months). Complete, partial, and stable response was achieved in 11 (65%), 4 (24%), and 2 (12%) of patients, respectively. Only one patient who received electron treatment for conjunctival MALT lymphoma developed local recurrence 47 months after boom-boom treatment. The patient was successfully salvaged with full dose radiation, 24 Gy in 12 fractions. 3 patients developed distant progression outside orbits. At 3 and 5 years, 100% of patients maintained local control of the treated orbit. Figure 1 is a sample case showing complete response after radiation treatment.
Radiation and medical oncologist follow-up recorded a 6% and 0% rate of CTCAE grade 1 and 2+ toxicities. However, among those with comprehensive ophthalmologist follow-up (n=15), 5 patients (33.3%) developed new complications, including dry eye, cataracts, and chorioretinal atrophy. There were no eyes with significant loss of BCVA after RT (Table 2)
Table 2
| Treatment and toxicity outcomes | N [%] |
|---|---|
| Treatment response (n=17) | |
| Complete response | 11 [65] |
| Partial response | 4 [24] |
| Stable disease | 2 [12] |
| Progressive disease | 0 [0] |
| Recurrence rate (n=17) | |
| Local | 1 [6] |
| Distant | 3 [18] |
| Systemic | 0 [0] |
| Oncologist reported toxicity (CTCAE) (n=17) | |
| Grade 0 | 16 [94] |
| Grade 1 | 1 [6] |
| Grade 2+ | 0 [0] |
| Ophthalmologist reported toxicity (n=15) | |
| Dry eyes | 3 [20] |
| Cataracts | 1 [6] |
| Glaucoma | 0 [0] |
| Radiation retinopathy | 0 [0] |
| Radiation papillopathy | 0 [0] |
| Radiation maculopathy | 0 [0] |
| Restrictive strabismus | 0 [0] |
| Chorioretinal atrophy | 1 [6] |
| BCVA change (15 evaluable patients) | |
| No change | 15 [100] |
| Loss | 0 [0] |
| Increase | 0 [0] |
CTCAE, Common Terminology Criteria for Adverse Events; BCVA, best-corrected visual acuity.
Discussion
In this study, we demonstrated excellent response rate and local control with moderate ocular toxicities using “boom-boom” RT for orbital lymphoma. Only 1 of 17 patients experienced local progression, who was successfully salvaged with full dose radiation. The ultimate 3- and 5-year local control rates are 100%. Other reports using low dose (4 Gy) radiation treatment showed similar local control success rates (7-11). We also showed with comprehensive ophthalmology follow-up, up to 33.3% of patients experienced some toxicities. However, they are mild and none had significant changes in vision.
Conventional external beam radiation with dose of 30–36 Gy has local control rates close to 100% (6,14,15). Due to toxicity concerns, efforts were made to investigate the efficacy of low dose (4 Gy) radiation regimen for orbital lymphoma. Although ultra-low-dose radiation in orbital lymphoma has not been extensively studied prospectively, low-dose RT has been demonstrated to be an effective treatment for indolent NHL (7-11,16). The FoRT trial sought to understand differences in local control and toxicity in indolent follicular and marginal zone lymphomas of various disease sites treated with 4 vs. 24 Gy. Although treatment with 4 Gy was deemed inferior to treatment with 24 Gy, 5-year local control rates of 70% vs. 90% suggest that nearly three quarters of patients are able to achieve durable local control with only 4 Gy. Toxicity was reduced in the 4 Gy cohort: at 12 weeks, 10% patients in the 4 Gy group, as compared to 24.4% of patients in the 24 Gy group, experienced grades 1–2 toxicities. Out of 648 sites, 35 were orbital follicular lymphomas, which have an overall lower radiation tolerance compared to other disease sites (16).
Stanford group first reported low-dose (4 Gy) regimen for 20 patients with 27 ocular adnexal lymphomas in 2013 (7). With a median follow-up of 26 months, 2-year freedom from regional relapse rate was 96% (7). Subsequently, several other groups reported their single institution experiences with favorable local control rates of 75–100%, consistent with our rate of 94% (7-11). In the study by Rehn, 45 patients with 52 orbital lesions treated with various radiation doses were studied (11). Patients receiving 4–6 Gy were categorized as receiving ultra-low-dose RT, 24–30.6 Gy as standard-dose RT, and >30.6 Gy as high-dose RT. In the whole cohort, 11% of the lesions were treated with ultra-low-dose RT, 33% with standard-dose RT, and 56% with high-dose RT (11). Different radiation dose had no significant effect on progression free survival or overall survival (11). Currently, there is only one prospective phase 2 trial evaluating the efficacy of low-dose (4 Gy) radiation for orbital indolent B-cell lymphomas (NCT02494700) (17). The preliminary result was presented in abstract form at the 2022 American Society for Radiation Oncology (ASTRO) Annual Meeting. The trial included 50 evaluable patients with stage I to stage IV orbital indolent B-cell lymphomas. In a planned subset analysis of patients with newly diagnosed stage I MALT lymphoma, researchers observed a 2-year local control rate of 91%. At 2-year evaluation, 95% of these patients had not experienced a distant recurrence of disease (2022 ASTRO annual meeting) (17).
With the ultra-low-dose radiation treatment, the ocular toxicities are significantly reduced compared to conventional radiation dose. In the study by Rehn, ultra-low-dose RT (4–6 Gy) was associated with a significantly lower rate of grade 2 late toxicities, as compared to standard dose (24–30.6 Gy) or high dose (>30.6 Gy), 0% vs. 6% and 31%, respectively (11). In a recent systemic review showed similar findings (6). In the published studies evaluating ultra-low-dose radiation, very low rate of patient patients experienced acute ocular side effects, as per CTCAE grading, from treatment (7-11). However, these studies had limited levels of ophthalmologic assessment. These studies’ toxicity rates align with our oncologist-reported toxicity of 6%, but the ophthalmologist-reported toxicity of 33.3% suggests there could be potentially underreported mild ocular toxicity. Our series highlights the potential discordance in documented toxicity between oncologists who use CTCAE grading from patient-reported complaints and ophthalmologists who use detailed ophthalmologic evaluations. This emphasizes the importance of ophthalmology involvement in the detection of ocular toxicities post-RT for indolent orbital lymphoma patients.
There are limitations worth noting in our study. This was a retrospective study, which is susceptible to its inherent biases. Our sample size is relatively small, but is in line with other reports given the rarity of orbital lymphoma (7-11). Some of the patients did not have formal ophthalmology follow up after radiation, this may affect the rates of low-grade ocular toxicities reported in our study. Our study has a median follow of 39 months. However, given the indolent nature of low-grade orbital lymphoma, long-term follow up is needed to confirm the sustainability of radiation treatment local control. Lastly, due to retrospective nature of the study, there is also potential patient selection bias by the treating physician. This is minimized though multidisciplinary tumor board discussion. However, there still may be bias due to patient selection.
Conclusions
In conclusion, our study demonstrates high rates of local control and potentially underreported rates of low-grade toxicity with ultra-low dose (4 Gy in 2 fractions) for patients with indolent orbital lymphoma. Future prospective studies on the utility of ultra-low-dose RT for orbital indolent lymphomas is warranted. Studies should also focus on ophthalmologic toxicity endpoints based on ophthalmologist assessment, along with the effectiveness of salvage radiotherapy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://cco.amegroups.com/article/view/10.21037/cco-22-84/rc
Data Sharing Statement: Available at https://cco.amegroups.com/article/view/10.21037/cco-22-84/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://cco.amegroups.com/article/view/10.21037/cco-22-84/coif). AB reports receiving consulting fees from Genzyme and Oncopeptides. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This retrospective case series study was approved by the Institutional Review Board of Thomas Jefferson University (IRB# 18D.480) and is in compliance with the tenets set by the Declaration of Helsinki (as revised in 2013) and the Health Insurance Portability and Accountability Act. Patient consent was granted to obtain pertinent health information.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Olsen TG, Heegaard S. Orbital lymphoma. Surv Ophthalmol 2019;64:45-66. [Crossref] [PubMed]
- Ahmed OM, Ma AK, Ahmed TM, et al. Epidemiology, outcomes, and prognostic factors of orbital lymphoma in the United States. Orbit 2020;39:397-402. [Crossref] [PubMed]
- Chung HU, Son JH. Ocular adnexal mucosa-associated lymphoid tissue lymphoma: a narrative review. J Yeungnam Med Sci 2022;39:3-11. [Crossref] [PubMed]
- Yahalom J, Illidge T, Specht L, et al. Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 2015;92:11-31. [Crossref] [PubMed]
- Illidge T, Specht L, Yahalom J, et al. Modern radiation therapy for nodal non-Hodgkin lymphoma-target definition and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 2014;89:49-58. [Crossref] [PubMed]
- Oktariana TP, Andriana A, Nugroho RS. The outcome of radiation therapy as a primary treatment in orbital lymphoma: a systematic review. Rep Pract Oncol Radiother 2022;27:724-33. [Crossref] [PubMed]
- Fasola CE, Jones JC, Huang DD, et al. Low-dose radiation therapy (2 Gy × 2) in the treatment of orbital lymphoma. Int J Radiat Oncol Biol Phys 2013;86:930-5. [Crossref] [PubMed]
- Pinnix CC, Dabaja BS, Milgrom SA, et al. Ultra-low-dose radiotherapy for definitive management of ocular adnexal B-cell lymphoma. Head Neck 2019;41:1546. [Crossref] [PubMed]
- König L, Stade R, Rieber J, et al. Radiotherapy of indolent orbital lymphomas: Two radiation concepts. Strahlenther Onkol 2016;192:414-21. [Crossref] [PubMed]
- Baron J, Wright CM, Lee DY, et al. Low-Dose Radiotherapy Versus Moderate-Dose Radiotherapy for the Treatment of Indolent Orbital Adnexal Lymphomas. Front Oncol 2021;11:716002. [Crossref] [PubMed]
- Rehn S, Elsayad K, Oertel M, et al. Radiotherapy Dose and Volume De-escalation in Ocular Adnexal Lymphoma. Anticancer Res 2020;40:4041-6. [Crossref] [PubMed]
- de Castro B, Peixeiro RP, Mariz JM, et al. Ultra-low dose radiotherapy in the management of low-grade orbital lymphomas. Rep Pract Oncol Radiother 2022;27:467-73. [Crossref] [PubMed]
- Lee MJ, Lee MY, Choe JY, et al. Ultra-low-dose radiation treatment for early-stage ocular adnexal MALT lymphoma. Eur J Ophthalmol 2022;32:3092-6. [Crossref] [PubMed]
- Platt S, Al Zahrani Y, Singh N, et al. Extranodal Marginal Zone Lymphoma of Ocular Adnexa: Outcomes following Radiation Therapy. Ocul Oncol Pathol 2017;3:181-7. [Crossref] [PubMed]
- Pereira-Da Silva MV, Di Nicola ML, Altomare F, et al. Radiation therapy for primary orbital and ocular adnexal lymphoma. Clin Transl Radiat Oncol 2022;38:15-20. [Crossref] [PubMed]
- Hoskin PJ, Kirkwood AA, Popova B, et al. 4 Gy versus 24 Gy radiotherapy for patients with indolent lymphoma (FORT): a randomised phase 3 non-inferiority trial. Lancet Oncol 2014;15:457-63. [Crossref] [PubMed]
- Pinnix CC, Dabaja B, Gunther JR. Response adapted ultra low dose radiation therapy for the definitive management of orbital indolent B-cell lymphoma. Int J Radiat Oncol Biol Phys 2022;114:S2-3. [Crossref]


