Biomarker-based trials in neuro-oncology
Introduction
The treatment of patients with primary brain tumors has been and remains challenging. Initially, all primary brain tumors were treated similarly, as differences among the tumors were either not recognized or were ignored because there were no alternative treatment options to offer to patients with different types of tumors. Over the years, actionable differences among primary brain tumors have been identified. The first distinctions were made on the macro level through histopathology differences. The current World Health Organization (WHO) classification system of primary brain tumors (4th ed., 2007) is based on morphologic criteria (1). The majority of malignant gliomas are classified as infiltrating tumors, which include diffuse astrocytoma (grade II), anaplastic astrocytoma (grade III), oligodendroglioma (grade II), anaplastic oligodendroglioma (AO) (grade III), primary glioblastoma (GBM) (grade IV), and secondary GBM (grade IV). Primary GBM arises de novo without evidence of progression from a lower grade tumor whereas secondary GBM arises from an initially lower grade lesion. GBM is the most aggressive form of primary brain tumor and represents the majority of malignant primary brain tumors, with overall 5-year survival rates of less than 5% (2). Although most patients with any type of malignant primary tumor eventually succumb to their disease, patients with lower grade tumors have a better prognosis with median survival on the order of 2 to 6 years (3) for AOs and longer for grade II oligodendrogliomas.
It has been recognized that there is a range of clinical outcomes within each WHO class of primary brain tumor. Recently, there is accumulating evidence that tumors with similar histology have distinct molecular signatures associated with differences in survival. So far, most of the identified differences are based on prognostic markers, that is, markers that are associated with better or poorer outcomes independent of treatment. However, a few potential predictive biomarkers (biomarkers that selectively identify patients for whom a specific therapy may be effective) have been identified in the last several years. Newly discovered molecular signatures have the potential to become targets for current and future drug development. Clinical trials for these drugs have and will involve biomarkers. This article will review the history of biomarkers in clinical trials for brain tumors, will describe current trials, and will describe the likely design of trials to open in the next couple of years. The focus will be on higher-grade gliomas (GBMs and AOs) because other brain tumor types are relatively rare with less data available. This review is not meant to be comprehensive but rather to serve as an overview of biomarker-based clinical trials for primary malignant brain tumors.
Historical trials
The mainstay of treatment for malignant brain tumors has been surgical resection of as much of the tumor as possible. In some cases, it is not possible to resect the tumor because of its location within the brain. Until the 1970s, the benefit of radiotherapy (RT) for the treatment of malignant brain tumors was unclear. The Brain Tumor Study Group conducted randomized multi-institution trials that demonstrated that RT prolonged survival of patients with primary brain tumors (4,5). All types of malignant brain tumors were allowed on these trials but most patients had GBMs or other high grade tumors. At that time, the idea that oligodendrogliomas were a kind of separate disease was not formulated (6). These trials were conducted on an unselected population of patients and did not incorporate a biomarker. However, they provided the basis for RT as a standard adjuvant therapy for all patients with high-grade gliomas, including AOs.
The potential role of chemotherapy in malignant brain tumors was also not clear at that time. In the Brain Tumor Study Group trials mentioned above, the addition of chemotherapy to RT increased the proportion of patients with longer term survival but did not increase median survival (4,5). In the US, most neuro-oncologists recommended adjuvant chemotherapy with RT for high-grade tumors, especially GBMs. They felt that administering chemotherapy to all was justified in order to help a few patients live longer. However in other parts of the world, it was felt that the risks of chemotherapy outweighed the benefits (6). In the 1980s, the issue of exploring treatment options by histological type began. In particular, separate trials started being performed for GBMs and for high-grade oligodendrogliomas. Separate trials were also initiated for low-grade malignant brain tumors. In some sense, brain tumor histology was being used as an enrichment biomarker, where different trials were conducted for the different histologic types.
Glioblastomas (GBMs)
There have been multiple failures of targeted agents in clinical trials in GBM, all of which were conducted in unselected patient populations. EGFR is overexpressed in up to 60% of GBMs (7,8). Several phase II trials were conducted in unselected patients using EGFR TKI drugs such as gefitinib and erlotinib in recurrent and newly diagnosed GBM. Although some responses were observed, the overall efficacy was minimal when compared to historical controls (9-12). Alterations in PTEN expression are frequent in GBMs (up to 65%), with PTEN mutations being present in 15% to 40% of primary GBM (13,14). Preclinical studies suggested that PTEN-deficient tumors show enhanced sensitivity to mTOR inhibition providing a rationale for a phase II clinic trials of temsirolimus. However, the efficacy results in the unselected patient were disappointing with no improvement of outcomes (15,16). There have been several other disappointing phase II results in unselected patient populations including imatinib (17,18) and vatalanib (19,20). Given the relatively small sample sizes of these trials and few responses, it is difficult to determine whether these trials failed because they were conducted in an unselected patient population or for some other reason.
The use of adjuvant chemotherapy with adjuvant RT in GBMs was settled in 2005 by the landmark phase III trial led by the European Organization for Research and Treatment of Cancer (EORTC) and the National Cancer Institute of Canada (NCIC). This trial demonstrated prolonged overall survival (OS) for patients treated with adjuvant temozolomide (TMZ) chemotherapy in combination with RT followed by adjuvant TMZ compared to patients treated with adjuvant RT alone (21). This trial included only GBM patients and did not incorporate biomarker; it was performed in an unselected group of GMB patients. The current standard of treatment in GBM patients is surgery with concurrent RT with TMZ followed by adjuvant TMZ.
Anaplastic oligodendrogliomas (AOs)
Retrospective analyses and case series of patients indicated that AO tumors appeared responsive to chemotherapy (22,23) with high-grade oligodendroglioma patients receiving the combination of procarbazine, lomustine, and vincristine (PCV). This observation was confirmed in a prospective phase II study conducted by NCIC, which demonstrated a 75% response rate in AO patients treated with PCV (24). These results provided the basis for two Phase III trials: one led by the Radiation Therapy Oncology Group (RTOG 9402) and the other lead by EORTC, EORTC 26951. These two trials addressed the same question: does the addition of PCV to adjuvant RT improve outcomes compared to adjuvant RT alone (standard of care) for patients with newly diagnosed high-grade oligodendrogliomas. The timing and dose of PCV differed between the two trials. However, the initial reports of both trials were consistent: the addition of PCV significantly prolonged progression-free survival (PFS) but not OS (25,26). The lack of OS benefit for the entire trial cohort was also observed after longer follow-up in the RTOG 9402 trial (27); however after longer follow-up in EORTC 26951, patients treated with adjuvant PCV and RT had longer median survival versus patients treated with adjuvant RT alone (28). Note that these trials also did not use biomarkers as part of the design other than limiting the trial to high-grade oligodendroglioma patients.
Recent and current trials
Glioblastomas (GBMs)
A retrospective correlative analysis was performed on patients with tissue available from the landmark phase III EORTC/NCIC trial of TMZ, in which the association of methylation of O-6-methylguanine-DNA methyltransferase (MGMT) on patient survival was evaluated. The initial publication reported a statistically significant survival difference favoring chemoradiotherapy in patients with MGMT methylated tumors but a non-significant difference between the treatment arms for patients with unmethylated tumors (29). This suggested that MGMT methylation status is potentially a predictive biomarker of response to TMZ in GBM tumors. However, after longer follow-up, there was a statistically significant difference between treatment arms for both the methylated and unmethylated tumors, with a larger magnitude of benefit for patients with methylated tumors (30). This suggested that MGMT status is both prognostic as well as predictive (i.e., a quantitative predictive biomarker, where both biomarker groups benefit but the MGMT-methylated group benefits more). Recently, two studies comparing radiation therapy to TMZ chemotherapy for the treatment of high-grade brain tumors in elderly patients indicate MGMT status is predictive: patients with methylated MGMT tumors had better outcomes when treated with TMZ than patients with unmethylated tumors, and for patients treated with radiation alone, there was no difference in outcome based on the MGMT methylation status of their tumors (31,32). At this time, it has not been definitively decided if MGMT methylation status is a predictive biomarker or not.
The ongoing NCIC CE.6 trial is assessing the MGMT methylation status in frail elderly patients randomized to a short course radiation therapy concurrent with TMZ versus a short course radiation therapy. This trial has completed accrual and is awaiting data maturation. All patients in the trial will have MGMT status assessed, although this was not done at the time of patient registration. The trial was powered to detect an OS difference between the treatment arms. The analysis of the MGMT status and treatment arm will be done as a correlative study with the intent to determine if there is an interaction between MGMT status and treatment (TMZ versus no TMZ). This is an informal biomarker-treatment interaction design because the study protocol does not specify formal testing to determine whether there are treatment differences in the MGMT-methylated group versus the MGMT-unmethylated group and the trial was not powered to detect an interaction between MGMT status and treatment. If MGMT status-by-treatment arm interaction term is significant, this will provide evidence that MGMT status is predictive of TMZ benefit in elderly patients. Further follow-up analyses would be needed to determine if the interaction is quantitative (there is a significant treatment effect for both MGMT methylated and unmethylated groups but the benefit is larger in the methylated group) or qualitative (the treatment effect is significant only for the MGMT methylated group). If the MGMT methylation status-by-treatment interaction term is not statistically significant, little information may be gained as to whether MGMT methylation is predictive or not because the study was not powered for the interaction.
Although there is no definitive data regarding whether MGMT methylation status is a predictive biomarker, there have been several enrichment design trials for GBMs launched on the basis of MGMT methylation status. A randomized phase III trial (cilengitide, TMZ, and radiation therapy in treating patients with newly diagnosed GBM and methylated gene promoter status, CENTRIC) was undertaken for newly diagnosed MGMT-methylated GBM that compared RT and TMZ (standard of therapy) to RT and TMZ plus cilengitide. The trial did not show a statistical significant survival advantage of the addition of cilengitide to the standard adjuvant therapy despite an encouraging median OS of 26 months (33).
The Alliance trial A071102 is a phase II/III trial comparing adjuvant veliparib (a PARP inhibitor) plus TMZ to adjuvant TMZ administered after the completion of surgery followed by concurrent radiation and TMZ in newly diagnosed GBM patients. This trial design is an enrichment design where MGMT methylation is an integral biomarker. Eligible GBM patients are pre-registered after surgery and their tumors are centrally tested for MGMT methylation status while they undergo treatment with concurrent radiation and TMZ (standard treatment). Patients identified as having tumors with MGMT methylation are randomized to continue treatment either with veliparib plus TMZ or with TMZ alone. Patients who have tumors that are MGMT unmethylated go off study. The phase II endpoint is PFS and the phase III endpoint is OS; the phase II patients will be used for the phase III endpoint analysis. At the completion of the phase II portion, the decision to continue accrual for the phase III trial will be based on the PFS HR (if after 121 PFS events are observed the PFS HR is 0.86 or greater, the phase III portion will not be completed), and the results of an interim analysis for OS (if after 160 deaths the OS HR is 0.875 or greater, the phase III portion will not be completed). The basis for using an enrichment design was the studies mentioned above showing potentially greater benefit of TMZ treatment in GBM patients with MGMT methylated tumors and strong-preclinical data of the additive effect of veliparib with TMZ in patients with MGMT methylated tumors (34-37), including unpublished preliminary data included in the protocol. Since it has not been definitively established that MGMT methylation status is a predictive biomarker for TMZ, the downside of using the enrichment design is that it will provide no information regarding the impact of adding veliparib to TMZ in patients with MGMT unmethylated tumors. It could even be the case that the combination might not be effective for patients with MGMT methylated tumors but is effective for patients with MGMT unmethylated tumors even though the pre-clinical data indicate this is unlikely.
There also have been trials undertaken in patients with newly diagnosed MGMT-unmethylated tumors. The CORE (cilengitide, TMZ, and radiation therapy in treating patients with newly diagnosed GBM and unmethylated gene promoter status) trial was a randomized phase II companion trial to CENTRIC (described above). This trial compared the addition of cilengitide to TMZ and radiation (two arms each with a different dose schedule for cilengitide) to the standard TMZ and radiation. There was no survival benefit observed for the addition of cilengitide (38). There also have been trial designs that tested regimens that did not use adjuvant TMZ in newly diagnosed GBM patients with MGMT-unmethylated tumors. These trials occurred outside of the US because treatment with adjuvant TMZ has become a standard of care within the US. The first trial was a single arm phase II trial that investigated the activity of adjuvant concurrent enzastaurin and RT (S039). The study failed to meet its pre-defined efficacy endpoint but the results suggested that omission of TMZ in this patient population may be ethically justified (39). Other trials for patients with newly diagnosed GBM that are MGMT-unmethylated include the GLARIUS (a study of bevacizumab (BEV) and irinotecan versus TMZ radiochemistry in patients with GBM) randomized phase II trial, which met its pre-defined efficacy endpoint (40), and EORTC 26092 randomized phase II trial, which did not meet its pre-defined efficacy endpoint (41).
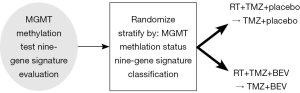
A current treatment by biomarker interaction design is being used in RTOG 0825 to evaluate the predictive value of GBM subtypes. In particular, RTOG 0825 is a phase III trial of TMZ and radiation with or without BEV for patients with newly diagnosed GBM (see schema in Figure 1). The primary analysis is a comparison of the two treatment arms with respect to a composite endpoint of PFS and OS. The study is powered for this analysis. Specifically, the trial has 80% power to detect a HR of 0.75 or less for OS (with one-sided significance of 0.023) and/or to detect a HR of 0.70 or less for PFS (with one-sided significance of 0.002); the trial will be positive if either or both of the OS and PFS criteria are met. The planned sample size is 612 eligible patients. Secondary analyses are planned to determine whether a nine-gene signature (42) is predictive of BEV response and whether MGMT methylation status is predictive of BEV response. It is hypothesized that the nine-gene signature may be predictive because it identifies angiogenesis enriched tumors. This trial will measure MGMT-methylation status and the nine-gene signature on all patients and has patients treated and not treated with BEV, thus following the so-called treatment by marker interaction design for the secondary objectives. However, the study is not formally powered to detect the treatment by biomarker interactions. The secondary biomarker hypotheses to be tested are: (I) that the nine-gene signature classification into “favorable” and “unfavorable” groups is prognostic for OS; and (II) the nine-gene signature classification into “favorable” and “unfavorable” groups is predictive of BEV benefit. There is adequate power to detect large prognostic effects (HR of 1.5 or greater) and limited power for determining whether it is predictive. Since MGMT status is collected on all patients, it can be determined whether it is predictive of BEV response, which the investigators propose to do; however the study was not powered to detect the interaction. Finally, the investigators also propose compare OS and PFS among the four different groups of patients determined by MGMT methylation status (methylated versus unmethylated) and nine-gene signature (favorable versus not favorable).
About 25% of primary GBMs have an EGFRvIII mutation, which is regarded as an important oncogenic mutation. As mentioned above, EGFR-targeted approaches in unselected GBM patient populations have not been found to be efficacious. However there is continuing effort to targeted EGFR treatments through the use of enrichment designs. One such effort is vaccination strategies for EGFRvIII-positive GBM tumors that target an epitope created by the mutation. Currently there have been promising results in phase II trials for the vaccine (43,44). A placebo-controlled, randomized, phase III enrichment design trial (ACT IV) for patients with GBM tumors that harbor an EGFRvIII mutation is underway to determine the efficacy of the EGFRvIII-directed vaccine (ClinicalTrials.gov, number NCT 10408479).
Anaplastic oligodendrogliomas (AOs)
As mentioned above, there were two large randomized trials RTOG 9402 and EORTC/NCIC 26951, completed that compared PCV in combination with radiation therapy to radiation therapy alone in patients with anaplastic oligodendroglial tumors. Upon a retrospective analysis of tumor tissue from study participants, both studies independently found 1p/19q co-deletion to be associated with PFS and OS. This marker appeared predictive of better PFS for patients treated with PCV but not predictive of OS benefit in the initial analyses (25,26). However, after longer follow-up, both trials demonstrated that survival was significantly longer in patients with 1p/19q co-deleted tumors treated with PCV plus radiation compared to patients with tumors that were co-deleted with radiation alone (27,28). No significant survival differences were seen between the two treatment arms for patients with tumors that were not 1p/19q co-deleted. Although the interaction term for the 1p/19q deletion status and treatment arm did not achieve statistical significance, the consistency of the results of both trials represented compelling evidence that 1p/19q deletion status is a predictive marker of chemotherapy (PCV) response and is accepted by most of the neuro-oncology community as such. To date, this is the only predictive biomarker in neuro-oncology that has been demonstrated in multiple phase III trials. These results led to two recent biomarker enrichment design phase III trials for high-grade oligodendrogliomas, which were designed as companion trials: the CATNON trial (ClinicalTrials.gov number NCT00626990; EORTC 26053/22054, RTOG 0834) and the CODEL trial (ClinicalTrials.gov number NCT00887146; NCCTG/Alliance N0577. Table 1 provides details of the two trials.
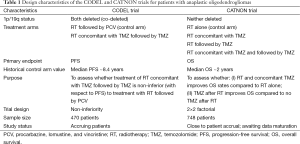
Full table
Near future trial designs
It has been recognized that brain tumors are heterogeneous in histology, genetic drivers, and outcome. Over the past decade, there has been substantial progress made identifying molecular characteristics of brain tumors. In particular, new mutations affecting IDH1, IDH2, H3f3, ATRX and CIC have allowed subclassification of gliomas into distinct molecular subgroups that have similar outcomes. However, none of the have been shown to predict patient benefit from therapeutic interventions; in other words, they are prognostic and not predictive. The first classification of GBMs based on gene expression profiling was reported in 2006 by Phillips and colleagues (45). They proposed new subtypes: proneural, proliferative, and mesenchymal. Much subsequent work has been done including the development of the nine gene signature by RTOG being tested in RTOG 0825 as mentioned above. The latest development is a classification of gliomas into five groups on the basis of three tumor markers: 1p/19q co-deletion status, IDH mutation, and TERT promotor mutations. The groups have different ages of onset, OS, and associations with germline variants characterized by distinct mechanisms of pathogenesis (46). There are associations of these classes with the current WHO classification: i.e., triple positive tumors that have all three mutations are strongly associated with oligodendroglial histology and GBMS are associated with TERT only mutations. It may be the case that the WHO classification may be replaced with molecular subtypes or at least supplemented with molecular information. This would impact eligibility criteria for future clinical trials in that they would be enriched for molecular subclasses rather than histologic subtypes.
Future trial designs of phase III trials will likely continue to be enrichment designs that arise from phase II trials that are done in all marker subgroups and identify the study subgroup and treatments to be tested in a phase III trial. Specifically, the next generation of phase II trials in newly diagnosed GBM will likely be adaptive screening trials similar to I-SPY 2 (Investigation of Serial Studies to Predict Your Therapeutic Response with Imaging and Molecular Analysis 2) (47). In such a trial, all patient tumors are genotyped and patients are randomized among a control arm and several experimental arms. The decision to drop an experimental arm and replace it with a new arm will be made if the predicted probability of success of that arm drops below a pre-defined threshold. Similarly, an arm would be dropped and recommended for phase III testing if the predicted probability of success is higher than a predefined threshold. The randomization schedule could either be fixed or adaptive in the sense that randomization probabilities are altered so that genetic aberration and treatment combinations that have had better outcomes get are given a higher randomization probability. Such a trial is currently being planned by the Alliance adult cooperative group (A071403) for patients with newly diagnosed GBM. The control arm would be standard of care after surgery: TMZ given concurrently with radiation followed by adjuvant TMZ. The experimental arms would be radiation and TMZ followed by the experimental drug or radiation and the drug followed by adjuvant drug. At this time there are three drugs of interest, each targeting a different aberration: RB-proficient tumors, EGFR amplified/mutated tumors, and PI3K/Akt/mTOR signaling pathway mutated tumors. Drugs are selected based on pre-clinical and clinical data demonstrating the ability to impact at least one of the aberrations of interest, demonstrated ability of the drug to cross the blood-brain barrier in humans, and ability to enhance radiation effects (this will determine whether the drug versus TMZ is given concurrently with radiation). Drug-genetic aberration combinations that cross the threshold for the probability of success would be tested in a phase III enrichment design trial of the drug containing regimen versus control (radiation concurrent with TMZ followed by adjuvant TMZ) for patients who have specific genetic aberration.
There are no immediate plans for the next trial in AO given that CATNON just closed and the data are currently several years from maturation and CODEL is actively accruing patients. However, it is likely that future trials will be enrichment designs based on 1p/19q co-deletion status or a refinement of this such as the triple-positive tumors mentioned above.
Summary
The progress of treatment advances in brain tumors has been distressingly slow. The first major advance was in the 1970s with the use of radiation after surgery. The next advance required over thirty years with the addition of TMZ to radiation for GBMs and PCV to radiation for anaplastic oligodengrogliomas. Although the molecular characterization of brain tumors have identified prognostic subgroups and targets, to date no targeted agent has been demonstrated to be efficacious in brain tumors. This may be due many reasons that include testing targeted agents in unselected patient populations, the agents did not adequately cross the blood brain barrier, or the microenvironment of brain tumors versus other solid tumors in which the targeted agents did work. Trials moving forward will likely continue to be enrichment designs due to the relatively small patient population of brain tumor patients available for clinical trials that make the conduct of marker by treatment interaction trials infeasible. The use of smarter randomized phase II designs to identify drug/tumor genetic combinations will be used to launch phase III enrichment trials that will hopefully have a higher likelihood of success.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007;114:97-109. [PubMed]
- Olar A, Aldape KD. Biomarkers classification and therapeutic decision-making for malignant gliomas. Curr Treat Options Oncol 2012;13:417-36. [PubMed]
- Anderson MD, Gilbert MR. Clinical discussion of the management of anaplastic oligodendroglioma/oligoastrocytoma (both codeleted and nondeleted). J Natl Compr Canc Netw 2014;12:665-72. [PubMed]
- Walker MD, Alexander E Jr, Hunt WE, et al. Evaluation of BCNU and/or radiotherapy in the treatment of anaplastic gliomas. A cooperative clinical trial. J Neurosurg 1978;49:333-43. [PubMed]
- Walker MD, Green SB, Byar DP, et al. Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med 1980;303:1323-9. [PubMed]
- Lassman AB. Success at last: a molecular factor that informs treatment. Curr Oncol Rep 2013;15:47-55. [PubMed]
- Nathoo N, Goldlust S, Vogelbaum MA. Epidermal growth factor receptor antagonists: novel therapy for the treatment of high-grade gliomas. Neurosurgery 2004;54:1480-8; discussion 1488-9. [PubMed]
- Heimberger AB, Hlatky R, Suki D, et al. Prognostic effect of epidermal growth factor receptor and EGFRvIII in glioblastoma multiforme patients. Clin Cancer Res 2005;11:1462-6. [PubMed]
- Rich JN, Reardon DA, Peery T, et al. Phase II trial of gefitinib in recurrent glioblastoma. J Clin Oncol 2004;22:133-42. [PubMed]
- Franceschi E, Cavallo G, Lonardi S, et al. Gefitinib in patients with progressive high-grade gliomas: a multicentre phase II study by Gruppo Italiano Cooperativo di Neuro-Oncologia (GICNO). Br J Cancer 2007;96:1047-51. [PubMed]
- Uhm JH, Ballman KV, Wu W, et al. Phase II evaluation of gefitinib in patients with newly diagnosed Grade 4 astrocytoma: Mayo/North Central Cancer Treatment Group Study N0074. Int J Radiat Oncol Biol Phys 2011;80:347-53. [PubMed]
- Raizer JJ, Abrey LE, Lassman AB, et al. A phase II trial of erlotinib in patients with recurrent malignant gliomas and nonprogressive glioblastoma multiforme postradiation therapy. Neuro Oncol 2010;12:95-103. [PubMed]
- Wang SI, Puc J, Li J, et al. Somatic mutations of PTEN in glioblastoma multiforme. Cancer Res 1997;57:4183-6. [PubMed]
- Zhou XP, Li YJ, Hoang-Xuan K, et al. Mutational analysis of the PTEN gene in gliomas: molecular and pathological correlations. Int J Cancer 1999;84:150-4. [PubMed]
- Galanis E, Buckner JC, Maurer MJ, et al. Phase II trial of temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group Study. J Clin Oncol 2005;23:5294-304. [PubMed]
- Chang SM, Wen P, Cloughesy T, et al. Phase II study of CCI-779 in patients with recurrent glioblastoma multiforme. Invest New Drugs 2005;23:357-61. [PubMed]
- Raymond E, Brandes AA, Dittrich C, et al. Phase II study of imatinib in patients with recurrent gliomas of various histologies: a European Organisation for Research and Treatment of Cancer Brain Tumor Group Study. J Clin Oncol 2008;26:4659-65. [PubMed]
- Wen PY, Yung WK, Lamborn KR, et al. Phase I/II study of imatinib mesylate for recurrent malignant gliomas: North American Brain Tumor Consortium Study 99-08. Clin Cancer Res 2006;12:4899-907. [PubMed]
- Conrad C, Friedman H, Reardon D, et al. A phase I/II trial of single-agent PTK 787/ZK 222584 (PTK/ZK), a novel, oral angiogenesis inhibitor, in patients with recurrent glioblastoma multiforme (GBM). J Clin Oncol 2004;22:abstr 1512.
- Reardon D, Friedman H, Yung WK, et al. A phase I/II trial of PTK787/ZK 222584 (PTK/ZK), a novel, oral angiogenesis inhibitor, in combination with either temazolomide or lomustine for patients with recurrent glioblastoma multiforme (GBM). J Clin Oncol 2004;22:abstr 1513.
- Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005;352:987-96. [PubMed]
- Cairncross JG, Macdonald DR. Successful chemotherapy for recurrent malignant oligodendroglioma. Ann Neurol 1988;23:360-4. [PubMed]
- Levin VA, Edwards MS, Wright DC, et al. Modified procarbazine, CCNU, and vincristine (PCV 3) combination chemotherapy in the treatment of malignant brain tumors. Cancer Treat Rep 1980;64:237-44. [PubMed]
- Cairncross G, Macdonald D, Ludwin S, et al. Chemotherapy for anaplastic oligodendroglioma. National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 1994;12:2013-21. [PubMed]
- Intergroup Radiation Therapy Oncology Group Trial 9402, Cairncross G, Berkey B, et al. Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: Intergroup Radiation Therapy Oncology Group Trial 9402. J Clin Oncol 2006;24:2707-14.
- van den Bent MJ, Carpentier AF, Brandes AA, et al. Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European Organisation for Research and Treatment of Cancer phase III trial. J Clin Oncol 2006;24:2715-22. [PubMed]
- Cairncross G, Wang M, Shaw E, et al. Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol 2013;31:337-43. [PubMed]
- van den Bent MJ, Brandes AA, Taphoorn MJ, et al. Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol 2013;31:344-50. [PubMed]
- Hegi ME, Diserens AC, Gorlia T, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 2005;352:997-1003. [PubMed]
- Stupp R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009;10:459-66. [PubMed]
- Malmström A, Grønberg BH, Marosi C, et al. Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol 2012;13:916-26. [PubMed]
- Wick W, Platten M, Meisner C, et al. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol 2012;13:707-15. [PubMed]
- Stupp R, Hegi ME, Gorlia T, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071-22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol 2014;15:1100-8. [PubMed]
- Clarke MJ, Mulligan EA, Grogan PT, et al. Effective sensitization of temozolomide by ABT-888 is lost with development of temozolomide resistance in glioblastoma xenograft lines. Mol Cancer Ther 2009;8:407-14. [PubMed]
- Carlson BL, Grogan PT, Mladek AC, et al. Radiosensitizing effects of temozolomide observed in vivo only in a subset of O6-methylguanine-DNA methyltransferase methylated glioblastoma multiforme xenografts. Int J Radiat Oncol Biol Phys 2009;75:212-9. [PubMed]
- Kitange GJ, Carlson BL, Mladek AC, et al. Evaluation of MGMT promoter methylation status and correlation with temozolomide response in orthotopic glioblastoma xenograft model. J Neurooncol 2009;92:23-31. [PubMed]
- Kitange GJ, Carlson BL, Schroeder MA, et al. Induction of MGMT expression is associated with temozolomide resistance in glioblastoma xenografts. Neuro Oncol 2009;11:281-91. [PubMed]
- Nabors LB, Fink KL, Mikkelsen T, et al. Two cilengitide regimens in combination with standard treatment for patients with newly diagnosed glioblastoma and unmethylated MGMT gene promoter: results of the open-label, controlled, randomized phase II CORE study. Neuro Oncol 2015;17:708-17. [PubMed]
- Wick W, Steinbach JP, Platten M, et al. Enzastaurin before and concomitant with radiation therapy, followed by enzastaurin maintenance therapy, in patients with newly diagnosed glioblastoma without MGMT promoter hypermethylation. Neuro Oncol 2013;15:1405-12. [PubMed]
- Herrlinger U, Schafer N, Steinbach JP, et al. The Randomized, Multicenter Glarius Trial Investigating Bevacizumab/Irinotecan Vs Standard Temozolomide in Newly Diagnosed, Mgmt-Non-Methylated Glioblastoma Patients: Final Survival Results and Quality of Life. J Clin Oncol 2014;32:abstr 2042.
- Wick W, Gorlia T, Van den Bent M, et al. Radiation therapy and concurrent plus adjuvant temsirolimus (CCI-779) versus chemo-irradiation with temozolomide in newly diagnosed glioblastoma without methylation of the MGMT gene promoter. J Clin Oncol 2014;32:abstr 2003.
- Colman H, Zhang L, Sulman EP, et al. A multigene predictor of outcome in glioblastoma. Neuro Oncol 2010;12:49-57. [PubMed]
- Sampson JH, Heimberger AB, Archer GE, et al. Immunologic escape after prolonged progression-free survival with epidermal growth factor receptor variant III peptide vaccination in patients with newly diagnosed glioblastoma. J Clin Oncol 2010;28:4722-9. [PubMed]
- Sampson JH, Aldape KD, Archer GE, et al. Greater chemotherapy-induced lymphopenia enhances tumor-specific immune responses that eliminate EGFRvIII-expressing tumor cells in patients with glioblastoma. Neuro Oncol 2011;13:324-33. [PubMed]
- Phillips HS, Kharbanda S, Chen R, et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 2006;9:157-73. [PubMed]
- Eckel-Passow JE, Lachance DH, Molinaro AM, et al. Glioma Groups Based on 1p/19q, IDH, and TERT Promoter Mutations in Tumors. N Engl J Med 2015;372:2499-508. [PubMed]
- Generali D, Berruti A, Foroni C, et al. Molecular oncology and the neoadjuvant setting: the perfect blend for treatment personalization and clinical trial design. J Natl Cancer Inst Monogr 2011;2011:67-70.