Training and certification of the surgical oncologist
Introduction
Surgical Oncology is a unique medical specialty that combines the technical mastery of surgical intervention with the cognitive mastery of tumor biology, which forms the basis of oncologic decision-making. The successful training of the Surgical Oncologist produces an oncologist who specializes in the surgical treatment of the cancer patient, a process that requires a unique training paradigm. This article will review the evolution of surgical oncology training in the United States of America, including the development of a core curriculum and set of training standards and assessments, resulting in the recent specialty certification in Complex General Surgical Oncology (CGSO) by the American Board of Surgery.
History of surgical oncology training programs in the USA
Amongst the first documented surgical procedures in history were those performed for cancer, as recorded by the Edwin Smith Papyrus (1600 BC) and Ebers Papyrus (1550 BC) dating back to ancient Egypt (1). In fact, the evolution of surgery has largely been based on the imperative to treat tumors. It is therefore not surprising that cancer surgery and General Surgery were considered inseparable at the start of modern surgical residency training as proposed by William Halstead in 1889 (2). This model of surgical training was not questioned until the mid 1940’s when chemotherapy and radiation therapy started to prove effective as antineoplastic treatments. With the emergence of Medical Oncology and Radiation Oncology as medical specialties, there were some who started to consider tumor surgery as a specialty as well.
It was also at this time [1940] that the James Ewing Society was formed to honor Dr. James Ewing, the Memorial Hospital Pathologist and Oncologist who championed multidisciplinary care of the cancer patient. Dr. Ewing also served as Director of Memorial Hospital from 1931-1939. The Ewing Society also served as the Alumni Society for those who worked and trained at Memorial Hospital and became the precursor to the present day Society of Surgical Oncology (SSO), despite being a society open to all oncologic disciplines. As early as 1947, surgical trainees, under the James Ewing Society, performed unofficial specialty fellowships in Surgical Oncology at Memorial Hospital (Personal Communication: Okeefe K., 2014).
Over the next few decades, Surgical Oncology and unofficial fellowships in this discipline continued to grow. The first formal Division of Surgical Oncology in the United States was formed at the Medical College of Virginia in Richmond in the mid 1960’s (1). By the early 1970’s a debate developed amongst the leaders in the field of Surgical Oncology. Some surgeons wished to maintain and grow the existing James Ewing Society as the official society of the discipline while others wished to form a new academic surgical oncology society (Personal Communication: Balch C., 2014). In 1975, under President Edward Scanlon, M.D., the James Ewing Society transformed into the SSO (1).
The Society of Surgical Oncology (SSO)
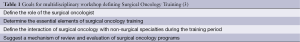
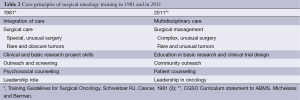
The newly formed SSO recognized that training future surgical oncologists was a top priority of the new society and the SSO Training Committee was formed to structure and organize fellowships under SSO oversight. Additionally, the SSO leadership recognized that a paradigm shift away from the surgical apprenticeship was necessary. In 1978 the SSO and the National Cancer Institute co-sponsored a workshop on graduate surgical oncology education in order to establish training guidelines for Surgical Oncology (3). The workshop included medical oncologists, pathologists, pediatric oncologists, gynecologic oncologists, representatives of the American Cancer Society and numerous surgical oncologists. The major goals for this workshop are outlined in Table 1. With a standardized set of goals and training guidelines in place and with oversight by the SSO Training Committee, fellowships in Surgical Oncology steadily grew. It is estimated that in 1986 there were 8 fellowships in the United States with 23 fellows finishing per year. By 1991 there were 11 fellowships, accounting for 30 fellows per year. In 1997 there were 12 fellowships and 32 fellowship positions. By 2008 there were 19 SSO approved fellowships (including 3 Canadian programs) accounting for 51 fellowship positions. At present there are 19 ACGME accredited fellowship programs (plus 3 Canadian programs receiving reciprocity for a total of 22 programs), accounting for 57 fellowship positions for the 2015 academic year.
The SSO Training Committee periodically undertook review and revision of the training standards and requirements over the past few decades, but the core principles remained similar. Table 2 reviews the elements of Surgical Oncology training based on the original SSO/NIH consensus conference in 1978 compared to the 2011 Complex General Surgical Oncology Curriculum Statement to the American Board of Medical Specialties. Despite changes in nomenclature, the basic tenets of Surgical Oncology training remain very much intact.
Full table
Fellowship match
As Surgical Oncology fellowships grew in number, there was need for a more standardized and objective way to distribute fellowship positions amongst qualified applicants. For years fellowship programs called their top applicants and offered them a position with a narrow timeline to either accept or decline. Applicants may not have heard yet from their top choices of programs yet, but would still be forced to decline or accept any offered position. The implementation of a standard algorithm for matching fellowship applicants to fellowship programs took place in the mid 1990’s under the Training Committee Leadership of Dr. Daniel Coit. The match was performed by the SSO Training Committee using a handmade spreadsheet for almost one decade until the SSO commissioned the computerization of its matching algorithm. The SSO computerized matching program was first used in 2004 and is still used for the Breast Oncology Fellowship match.
From 2009-2011, prior to the approval of the certificate in CGSO, the SSO matching program was used to match all Surgical Oncology, Hepatobiliary, and Breast fellowship positions. With the approval of CGSO certificate, the Surgical Oncology Fellowship matching process is now overseen by the National Residency Matching Program (NRMP).
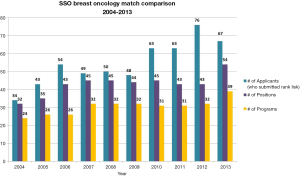
Breast Oncology Fellowships
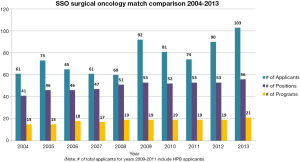
In 2002 the Executive Council of the SSO charged the SSO Training Committee (under the leadership of Dr. Scott Kurtzman) to develop an approval process for breast fellowship programs. This would be a tripartite fellowship initiated through a partnership between the SSO, the American Society of Breast Surgeons, and the American Society of Breast Disease in response to the tremendous advances in knowledge and treatments available for the breast cancer and breast disease patient. The development of a breast fellowship also recognized the growing number of surgeons whose clinical practice and research efforts were devoted to breast diseases. In 2003 the SSO Training Committee granted 33 programs conditional approval. The first match took place in 2004, with 24 programs participating and 32 fellowship positions available. In 2012 new program applications were accepted and a total of ten new breast programs were approved by the SSO Training Committee. Figure 1 demonstrates the evolution and continued growth of the Breast Oncology Fellowship match since the first match in 2004.
Certification process and the SSO
The desire to see Surgical Oncology receive recognition as a specialty within General Surgery has been expressed by some for decades. In fact, there were calls for a Board of Oncology under the oversight of the American Board of Surgery as early as the 1940’s. Dr. Fabrizio Michelassi, in his 2010 SSO Presidential Address, details the multi-decade effort to successfully achieve subspecialty certification in CGSO (4). The first nearly successful attempt at subspecialty recognition happened between 1984 and 1989. Although ultimately unsuccessful, the SSO was given the oversight of a Certificate of Added Qualification (Personal Communication: Balch C., 2014). In 1998 the Surgical Oncology Advisory Council (SOAC) of the American Board of Surgery was established. Numerous years of discussions and certain concessions followed and in June of 2009 the American Board of Surgery approved a subspecialty certificate in Advanced Surgical Oncology. On April 28, 2011 the American Board of Surgery announced a new certificate in CGSO and the Surgical Oncology Advisory Council became the Surgical Oncology Board (SOB) of the American Board of Surgery.
The American Board of Surgery is only able to grant certification to graduates of programs accredited by the Accreditation Council on Graduate Medical Education (ACGME). On June 10, 2012 the ACGME Board of Directors approved accreditation for CGSO programs. In the United States, the ACGME oversees all training programs for certified specialties and subspecialties. Of the 19 programs that had been approved by the SSO at the time of the establishment of CGSO, 16 were located in the USA. All 16 have earned ACGME accreditation (the ACGME does not certify Canadian programs). Three new US programs have applied for and received ACGME accreditation. To clarify, the ACGME is the regulatory body that accredits training programs (in this case, CGSO Fellowships). The American Board of Surgery oversees certification of individual surgeons (in this case the surgeon would need to be certified in General Surgery and then obtain specialty certification in CGSO).
CGSO curriculum development
In 2008, in preparation for CGSO certification by the American Board of Surgery, the Training Committee of the SSO undertook a strategic evaluation of the surgical oncology curriculum and existing requirements. The curriculum, as proposed to the American Board of Medical Specialties, was based on a two-year fellowship and the main components of the curriculum include instruction in (I) multidisciplinary care; (II) patient counseling; (III) surgical management of oncologic conditions; (IV) non-surgical cancer treatment modalities; (V) clinical research and trial design and (VI) community outreach.
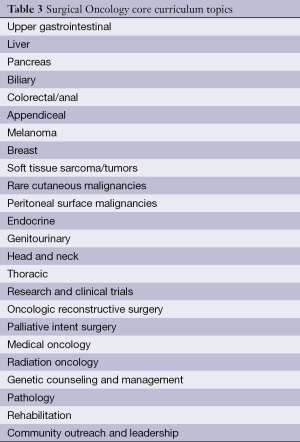
The newly revised core curriculum was modeled after the Surgical Council on Resident Education (SCORE) curriculum outline for General Surgery Residency. The Surgical Council on Resident Education is (5) “a nonprofit consortium formed in 2006 by the principal organizations involved in U.S. surgical education”, including The American Board of Surgery, The American College of Surgeons, The American Surgical Association, The Association of Program Directors in Surgery, The Association for Surgical Education, the Residency Review committee for Surgery of the ACGME, and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). The core topics covered by the surgical oncology core curriculum are outlined in Table 3.
Full table
The CGSO Core Curriculum was approved by the Executive Council of the SSO and recommended to the Residency Review Committee-Surgery (RRC-Surgery) of the ACGME to be used as a basis for the ACGME Program Requirements for CGSO fellowship. These requirements were drawn up by a task force that included members of the RRC-Surgery and a representative of the SSO. The two-year fellowship requires surgical rotations as well as non-surgical clinical rotations to stress the multidisciplinary nature of surgical oncology training. Additionally, training in unusual malignancies (peritoneal surface malignancies, regional disease, and rare cutaneous malignancies) is stressed as these are not typically encountered during General Surgery training. In addition to the surgical and non-surgical rotations, research and research training (including education in human and animal research protocols) are mandated parts of the fellowship, as is community outreach and training in assuming a leadership role in oncologic care.
The SOB of the American Board of Surgery has also approved the use of the SCORE-based Surgical Oncology Core Curriculum as the basis for examination development in CGSO. The first qualifying examination in CGSO took place in September 2014 and the first certifying examination is scheduled for February 2015. The SSO has taken the lead in developing educational materials for fellows preparing for the new CGSO examination and released the first edition of the Surgical Oncology Self-Assessment Program (SOSAP) in 2013.
Case volume and multidisciplinary experience
The Training Committee of the SSO also undertook evaluation of the index cases that it felt was essential to Surgical Oncology training. By collecting data from the majority of SSO approved training programs, the SSO calculated statistics on various surgical oncology cases. The SSO also proposed tracking multidisciplinary education in oncology to assure this critical aspect of the specialty is taught. At present, both the RRC-Surgery and the SOB of the American Board of Surgery are considering case volume and multidisciplinary requirements.
CGSO assessment
As mentioned above, the SOB of the American Board of Surgery has finalized both a qualifying (written) examination and certifying (oral) examination, both of which will be administered in the near future. These examinations will be used to determine the certification status of individual graduates of ACGME-accredited CGSO programs. The multidisciplinary nature of this specialty is a focus of these examinations. However, the emphasis on interdisciplinary care must also be reinforced and stressed during fellowship training. The Milestones Project for CGSO will help to assure this process.
The Milestones Project of the ACGME was intended to provide a framework for assessment of the development of a trainee in key dimensions of the elements of physician competency in a specialty. They are designed to help assess the domains of physician competency (6). During the development of CGSO milestones, an emphasis was placed on the interdisciplinary nature of Surgical Oncology. All CGSO fellows will be assessed for milestone achievement throughout their fellowship by their program directors and the Program’s Clinical Competency Committee.
Educational content to support CGSO trainees
As discussed earlier, the CGSO Core Curriculum was based on the SCORE model for General Surgery. In similar fashion, the SSO and the American Board of Surgery will partner in providing web-based educational content on the SCORE Web Portal based on the CGSO Core Curriculum. This web-based educational initiative by the American Board of Surgery is used by almost all U.S. based surgical residency programs for a standardized weekly educational curriculum that includes links to topic specific reading material, multiple choice quizzes, discussion-based questions, videos etc. The SSO, with the leadership of the newly formed SCORE Committee of the SSO, will partner with the SOB of the American Board of Surgery to author and host educational content. The intention is that this will provide a standard weekly educational curriculum for all CGSO programs and fellows. The Annals of Surgical Oncology will serve as a critical source of reading material for the fellows through the SCORE portal.
As noted above, another resource for CGSO fellows preparing for their certification examinations is SOSAP. This commercially available educational resource has been prepared by the SSO for both the CGSO trainee and for General Surgeons who have a significant practice involving Surgical Oncology.
Involvement with related specialties
The successful accreditation of CGSO has seen an increase in the number of applicants applying for CGSO fellowships (Figures 2,3). However, the SSO recognizes its leadership role within the greater oncologic and surgical community as it pertains to fellowship training. The SSO seeks to continue the possibility of future tracking within CGSO through continued conversations with the American Board of Surgery and ACGME as well as specialty societies such as Americas Hepato-Pancreato-Biliary Association (AHPBA), the American Association of Endocrine Surgeons (AAES), and the American Society of Breast Surgeons (ASBS). Furthermore, the SSO is actively engaged with other organizations to discuss the multiple mechanisms that exist for training in certain disease sites. For example, there is considerable overlap between the CGSO fellowship curriculum and Hepato-Pancreatico-Biliary fellowship curriculum. For this reason, the SSO will co-host a consensus conference on training in hepatobiliary surgery along with the AHPBA and the American Society of Transplant Surgeons. This conference will take place during the October 2014 American College of Surgeons Clinical Congress.

It is further recognized that the majority of surgical care of cancer patients in the USA, which encompasses the field of Surgical Oncology, is provided by General Surgeons who have not completed formal specialty fellowship training in Surgical Oncology. Providing a framework for continued educational opportunities and assessment of quality in surgical oncology care will require on-going efforts by the SSO and the American Board of Surgery.
The future
Continued advances in cancer biology, technology, and multidisciplinary oncology care have driven the evolution of training paradigms in Surgical Oncology. The SSO, through partnerships with the American Board of Surgery, the ACGME, and related subspecialty societies can help assure that the Surgical Oncologist assumes a leadership role in cancer care treatment, cancer research, and career-long education of the practicing cancer practitioner.
Acknowledgements
Authors’ Contribution: Drs. Berman and Weigel contributed to the article outline, content, preparation and review.
Disclosure: Dr. Weigel presently serves as the President of the Society of Surgical Oncology and Dr. Berman is past Chairman of the Training Committee and present Chairman of the SCORE Committee for the Society of Surgical Oncology. The authors declare no conflict of interest.
References
- Lawrence W Jr. History of surgical oncology. In: Norton JA, Barie PS, Bollinger RR, et al. eds. Surgery. Basic science and clinical evidence. New York: Springer, 2000:1889-900.
- Pellegrini CA. Surgical education in the United States: navigating the white waters. Ann Surg 2006;244:335-42. [PubMed]
- Schweitzer RJ, Edwards MH, Lawrence W Jr, et al. Training guidelines for surgical oncology. Cancer 1981;48:2336-40. [PubMed]
- Michelassi F. 2010 SSO presidential address: subspecialty certificate in advanced surgical oncology. Ann Surg Oncol 2010;17:3094-103. [PubMed]
- SCORE: Surgical Council on Resident Education. 2014 [updated 2014 July; cited 2014 Aug 4]. Available online: http://www.surgicalcore.org/
- The Complex General Surgical Oncology Milestones Project. 2014 [updated 2014 May; cited 2014 Aug 4]. Available online: https://www.acgme.org/acgmeweb/Portals/0/PDFs/Milestones/CGSO.pdf