
Guidelines for biliary stents and drains
Background
Malignant biliary obstruction is a stricture or narrowing of the bile ducts caused by a tumor.
Cholangiocarcinoma is one of two common cancers to cause malignant biliary obstruction (1). Patients with malignant biliary obstruction usually present with painless jaundice, icteric sclerae, dark urine, light or clay colored stools, and pruritus. Hepatobiliary and pancreatic cancers are often locally advanced or metastatic at initial diagnosis and curative resection is often not an option. Treatment of malignant biliary obstruction is primarily treated by biliary catheterization or stent placement (2). The usefulness of these procedures was evidenced in the Gemcitabine Cisplatin ABC 02 study in advanced biliary cancer by Valle et al. (3), where 45% of patients in each arm had stents and in the FOLFIRINOX study by Conroy (4) in pancreatic cancer where 25% of patients had stents.
Management strategies
There are several options to treat malignant biliary obstruction which are based on the goals of treatment. These include medical management, stent placement through endoscopy, percutaneous transhepatic biliary drains through interventional radiology, and surgical options (4). Biliary stenting and drainage through endoscopic retrograde cholangiography (ERCP) is the preferred method for both distal and more proximal biliary obstruction, and for patients who are not surgical candidates.
The prevalence of biliary stents or percutaneous transhepatic drainage (PTBD) catheters for patients with CCA was emphasized in Miyazaki clinical practice guidelines for the management of biliary tract cancers with a Grading of Recommendations, Assessment, Development and Evaluation system (GRADE) (5). The primary recommendation for preoperative biliary drainage for patients with jaundice is extended hepatectomy. Patients are often diagnosed with locally advanced or inoperative disease, or metastatic disease, prohibiting hepatectomy as an intervention (5). The treatment decision for management of malignant biliary obstruction includes input from medical oncologists, diagnostic radiologists, surgical oncologists, gastroenterologists, and interventional radiologists (2).
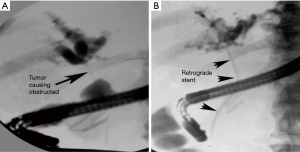
The procedure of choice to relieve biliary obstruction is ERCP (6). It is successful at 90% of the time (7). ERCP is preferable to initially attempt direct cholangiography (injection of contrast directly into the biliary tree) and stent placement, if a patient is able to tolerate it. The principle advantage of the retrograde approach is that no external drainage tube or bag is necessary leading to increased patient comfort and reduced impact on activities of daily living. Moreover, there is a reduction of procedural bleeding complications as a percutaneous transhepatic puncture is not required. Plastic stents may be placed as well as removable and non-removable self-expanding metallic stents and stent-grafts which can be placed by the endoscopic retrograde approach (Figures 1-3). However, there are anatomic situations in which an ERC cannot be performed. These anatomic situations are previous Roux-en-y gastric bypass, and previous surgical biliary bypass with the creation of a Roux-en-y hepato-jejunostomy (8). ERC may be unsuccessful due to inability to cannulate the biliary system secondary to factors such as: papillary distortion from tumor, obstruction of the duodenum, the presence of a duodenal diverticulum, or operator inexperience (6).
When ERCP is unsuccessful or not medically appropriate, PTBD is considered as the minimally invasive alternative procedure (9). Surgical biliary bypass may be an option in specific situations in which neither ERCP or PTBD can be performed. Percutaneous transhepatic biliary drainage for malignant biliary obstruction is concluded to be a safe and effective method to relieve jaundice caused by locally advanced cancers, when placing an ERCP is not possible (9). Additional treatment following biliary drainage includes surgery, chemotherapy and radiation. These are likely to increase patient survival (6).
Stents
Plastic stents have generally been recommended for patients with hepatobiliary and pancreatic cancers with a poor prognosis (10). A prospective trial by Wilcox et al. found that patients with a Karnofsky score of <80, or metastatic disease, showed a median survival of 2.8 months for patients with plastic stents (68.4%) and a median survival of 11.6 (31.6%) months for patients with uncovered self-expandable metal stents (SEMS). Ballard et al. performed a prospective study of 142 consecutive patients with resectable or borderline resectable pancreatic cancer with SEMS placed for biliary obstruction, who received neoadjuvant treatment (11). The median timepoint from SEMS placement to surgery was 110.5 days. During this time reintervention was necessary in 16 patients. By 282 days, reintervention was necessary in 21 patients (11). The authors concluded that SEMS provided more durable biliary drainage than plastic stents. In a study of 49 patients (12), Boulay et al. concluded plastic biliary stents don’t maintain patency during the time required for patients to complete neoadjuvant treatment for pancreatic cancer and SEMS may be safer and more cost effective in the long run (12). This was based on findings that only 22 patients had stents that remained patent throughout the course of treatment. Thirteen patients developed ascending cholangitis, and 14 had developed abnormal liver studies. A total of 17 patients required hospitalization. Plastic stents are less expensive, and a majority of non-academic medical centers utilize them (11).
Cholangitis is an uncommon but serious complication following ERCP (13). Symptoms include fever, jaundice, and right upper quadrant pain. In a retrospective chart review, Tierney et al. identified 57 of 431 patients who met the definition of post ERCP cholangitis (13). Repeat ERCP after initial placement of a metal stent occurred at a median of 140 and 80 days for plastic stents (13). Tierney et al. found that a cancer diagnosis and placement of multiple stents were the highest risk factors for developing post ERC cholangitis. They also found that hypoalbuminemia was a significant risk factor for stent occlusion and cholangitis (13). This includes patients with cachexia and malnutrition. Patient with advanced age were also at greater risk of developing cholangitis (13).
Care of the patient with stents
Oncology health care providers and nurses need to understand the following regarding stents:
- There are no external drainage bags making it less stressful and more convenient for patients.
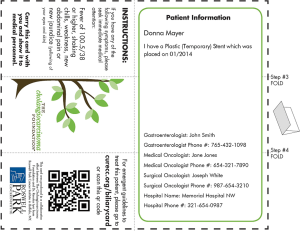
- A biliary emergency card or written information needs to be provided to the patient that includes the number of stents, type of stents (plastic or metal), the date of ERCP and stent insertion, and contact information for the gastroenterologist/endoscopist, and medical oncologist. The patient needs to be instructed to carry this information at all times and to present it to any medical providers (14).
- Fever greater than 100.4, chills, body aches, abdominal pain, sepsis, jaundice raises the possibility of stent occlusion and needs to be reported immediately. Replacement requires a repeat endoscopic procedure (usually general anesthesia).
- Retrograde stent placement should be performed when anatomy is appropriate and expertise available.
If retrograde stenting is not possible due to anatomic or technical reasons, percutaneous transhepatic biliary drainage should be performed in symptomatic patients.
- Symptoms include jaundice, pruritus, fever and sepsis.
- Percutaneous biliary drainage may be provided by.
- External biliary drainage catheter.
- Internal-external biliary drainage catheter.
- Placement of a completely internal metallic stent.
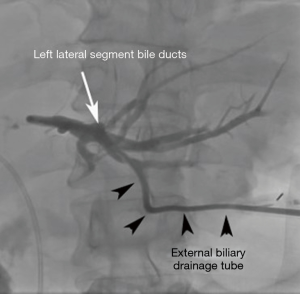
External percutaneous biliary drainage is accomplished by placing a catheter into the obstructed bile duct proximal to the obstruction. An external biliary drainage catheter must always be connected to an external drainage bag. If the bile stops flowing, the catheter should be flushed with 3 to 5 cc of sterile saline. If this is unsuccessful in restoring flow, the catheter may be occluded or displaced requiring replacement. Replacement is straight-forward and usually does not require general anesthesia.
Replacement of an external biliary drainage catheter can be accomplished with minimal analgesia and sedation as an outpatient. To replace the catheter, a guide wire is advanced through the existing catheter, and the existing catheter is removed leaving the guidewire in place. Subsequently a new drainage catheter is advanced over the guidewire securely into the obstructed duct. Appropriate tube position is confirmed by injecting and aspirating contrast media through the drainage tube. Most catheters have a locking “pigtail” loop at the tip, anchoring the drainage tube within the bowel. The pigtail is locked by pulling a suture that exits the catheter at or near the catheter hub.
Securing the catheter- The drainage catheter is secured by placing one or two tube anchoring sutures at the catheter entry site. In addition, specially designed adhesive dressings with manufactured tube fixation devices may be used. A sterile dressing is placed over the site.
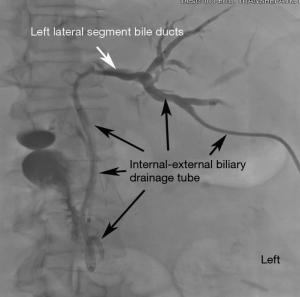
To place an internal-external drainage catheter, a guidewire is manipulated through the obstructing lesion into the distal unobstructed duct and distally into the duodenum. A specially designed catheter is ten advanced over the guidewire extending through the area of obstruction and into the bowel. The guidewire is then removed. These tubes are specially designed for percutaneous transhepatic biliary drainage and have multiple side holes created along the distal third of the tube. These side holes allow bile to flow from ducts proximal to the obstruction into the tube, through the tube, exiting the tube distal to the area of blockage.
Bile may drain into a bag or the catheter can be capped externally (no bag).
- Oncology health providers should expect.
- Continuous drainage of bile into the bag may be excessive (>1,000 cc/day) as duodenal contents will also drain through the tube when the tube is attached to a drainage bag. Providers need to be aware of the risk of dehydration from large amounts of biliary drainage. Patients require clear instructions for measuring drainage and capping the tube if having large amounts of drainage.
- The catheter should be routinely flushed with 3 to 5 cc of sterile saline daily.
- Dysfunction may be signaled by acholic stools, fever or jaundice.
- Replacement is straight-forward and usually does not require general anesthesia. Replacement can be performed as an outpatient with minimal analgesia and sedation over a guidewire under fluoroscopic guidance.
Advantages of percutaneous biliary drainage:
- Very high success rate, even when retrograde drainage fails.
- Easy replacement of problematic tubes without general anesthesia.
- Ability to confirm that bile is draining by intermittently connecting to bag (if internal-external).
Disadvantages of percutaneous biliary drainage:
- Requires an external catheter.
- Patients may take shower but cannot submerge the tube in water.
- Patient comfort.
- Nuisance of the bag when external drainage is performed.
- Mobility.
- Necessity of emptying the bag.
- Odor from the bag (remedied by changing to a new bag).
The major complications of percutaneous transhepatic cholangiography and biliary drainage are bleeding, infection and damage to surrounding structures.
Persistent bleeding is most often secondary to a hepatic arterial injury caused by the needle. The arterial injury may result in frank extravasation or the formation of a pseudoaneurysm. The bleeding can be into the bile ducts resulting in hemobilia and gastrointestinal hemorrhage or external to the liver leading to hemoperitoneum or hemothorax. Clinically, manifestations of hemorrhage include tachycardia, hypotension, abdominal pain, chest pain and shortness of breath.
Immediate resuscitative measures are required to treat clinically significant bleeding with replenishment of volume by transfusion of packed red blood cells, or administration of crystalloids when blood is not immediately available. Transfer to an intensive care unit and emergent angiography with embolization of the bleeding vessel is usually warranted. If emergent angiography is unsuccessful in controlling the hemorrhage, surgical intervention may be necessary, particularly if the bleeding is originating from an intercostal artery or diaphragmatic arterial branch. Unfortunately, surgical intervention is of limited use in controlling hemobilia, as this injury occurs deep within the hepatic parenchyma. Bleeding from a portal vein can generally be corrected by repositioning the drainage catheter so no side-holes are located within the hepatic parenchyma.
Percutaneous biliary drainage may also be complicated by sepsis following the procedure when the biliary system is infected at the time of drainage. Prophylactic antibiotics with broad spectrum coverage should be administered to all patients undergoing percutaneous biliary drainage. Overdistension of the biliary ductal system by injection of contrast media should always be avoided as this will often lead to sepsis. Bile duct stones are often associated with infected bile and particular caution should be exercised when performing biliary drainage in these patients. Medical management of post biliary drainage sepsis should include fluid resuscitation, antibiotics and pressors. Transfer to an intensive care unit is often required.
The following education instructions to the patient and caregiver for biliary drains and stents should be provided prior to discharge:
- The biliary system.
- Types of biliary drainage catheters/stents.
- External biliary drainage-catheter goes through the skin and into the bile ducts placed above the blockage, explain that catheter will come out of abdominal area into drainage bag (animation of blockage and tube going out into drainage bag).
- Internal-external biliary drainage-catheter goes through the skin and into the bile ducts across the blockage. One end of the catheter sits in the small intestine and other end come out through skin into drainage bag. Allows bile flow in 2 directions, either out to external collecting bag or into small intestine.
- Internal biliary drainage (stent) metal or plastic to hold the blocked area open. Plastic stents always require periodic replacement endoscopically.
- Before the procedure.
- Medications that will need to be discussed with the doctor before taking.
- Examples of specific medications, anti-coagulants, persantine, NSAIDS, diuretics and insulin.
- Previous allergic reaction to contrast dye.
- Instructions for eating and drinking before the procedure.
- After the procedure.
- Equipment that is specific to patient drains or stents.
- Explanation of the catheter, marking that helps detect if catheter has moved, disk and silicone disk against the skin.
- Explanation of the 3 way stopcock (if present), one port to drainage catheter, one port to the drainage bag and center port with needleless connector.
- Types of stents, proposed expected schedule for changes if needed.
- iv Instructions on completion of biliary emergency card (sample completed card, see Figure 4).
- Caring for the biliary catheter.
- Step by step instructions with actual equipment with instructor performing the following:
- Instructions for inspecting the catheter.
- Instructions for flushing the catheter with normal saline, as well as a schedule for flushing the catheter, if appropriate.
- Instructions for emptying the bag.
- Instructions for measuring and recording the color and amount of drainage with instructions on how to replenish fluids lost, recommended electrolyte replenishing drinks.
- Instructions for dressing change.
- Instructions for stopcock and drainage bag change.
- List of supplies they will need at home.
- Activities of daily living with biliary catheter.
- Instructions for showering, no bathing, swimming or submerging of catheter in water.
- Instructions for applying the protective covering.
- Instructions for dressing, no tugging on catheter, keep tubing secured to body with device.
- Precautions for work, travel and exercise.
- Routine change of biliary catheter proposed schedule.
- Instructions for capped biliary drainage catheter with symptoms to watch for post capped.
- When to call the nurse or doctor for signs and symptoms.
- Temperature of 100.4 F or higher.
- The amount of drainage has decreased greatly or stopped.
- Drainage is red with blood.
- Leaking fluid around insertion site.
- Location of marking for catheter has changed.
- Kink in tubing that cannot straighten out.
- Pain, tenderness or swelling at catheter site.
- Skin around the catheter looks red or irritated.
- The presence of nausea.
- Ascites- swelling of the abdomen.
- The presence of dizziness when standing.
- New or increased jaundice.
In conclusion, biliary drainage in cholangiocarcinoma retrograde endoscopic stent placement is procedure of choice when anatomy suitable and expertise available. Most other patients should receive internal external drainage tubes, avoiding the necessity of a drainage bag. External drainage is used when obstruction cannot be crossed or to drain multiple segments with a single tube. Metal stents should be reserved for patients with anticipated survival rate of less than 4 months when biliary anatomy is appropriate. Some patients have such extensive obstructions that preclude percutaneous or endoscopic biliary drainage. Supportive and comfort care is most appropriate in these individuals.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Bergquist A, Von Seth F. Epidemiology of cholangiocarcinoma. Best Pract Res Clin Gastroenterol 2015;29:221-32. [Crossref] [PubMed]
- Lorenz JM. Management of malignant biliary obstruction. Semin Intervent Radiol 2016;33:259-67. [Crossref] [PubMed]
- Valle J, Wasan H, Palmer DH, et al. Cisplatin plus Gemcitabine versus Gemcitabine for biliary tract cancer. N Engl J Med 2010;362:1273-81. [Crossref] [PubMed]
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus Gemcitabine for Metastatic Pancreatic cancer. N Engl J Med 2011;364:1817-25. [Crossref] [PubMed]
- Miyazaki M, Yoshitomi H, Miyakawa S, et al. Clinical practice guidelines for the management of biliary tract cancers 2015, the 2nd English edition. J Hepatobiliary Pancreat Sci 2015;22:249-73. [Crossref] [PubMed]
- Khan MA, Akbar A, Baron TH, et al. Endoscopic Ultrasound-Guided Biliary Drainage: A Systematic Review and Meta-Analysis. Dig Dis Sci 2016;61:684-703. [Crossref] [PubMed]
- Ang TL, Teo EK, Fock KM. EUS-guided transduodenal biliary drainage in unresectable pancreatic cancer with obstructive jaundice. JOP 2007;8:438-43. [PubMed]
- Attasaranya S, Netinasunton N, Jongboonyanuparp T, et al. The Spectrum of Endoscopic Ultrasound Intervention in Biliary Diseases: A Single Center’s Experience. Gastroenterol Res Pract 2012;2012:680753. [Crossref] [PubMed]
- Moole H, Dharmapuri S, Duvvuri A, et al. Endoscopic versus Percutaneous Biliary Drainage in Palliation of Advanced Malignant Hilar Obstruction: A Meta-Analysis and Systematic Review. Can J Gastroenterol Hepatol 2016;2016:4726078. [Crossref] [PubMed]
- Wilcox CM, Kim H, Seay T, et al. Choice of plastic of metal stent for patients with jaundice with pancreaticobilary malignancy using simple tools: a prospective evaluation. BMJ Open Gastroenterol 2015;2:e000014. [Crossref] [PubMed]
- Ballard D, Rahman S, Ginnebaugh B, et al. Safety and efficacy of self-expandin metal stents for biliary drainage in patients receiving neoadjunvant therapy for pancreatic cancer. Endosc Int Open 2018;6:E714-21. [Crossref] [PubMed]
- Boulay BR, Gardner TB, Gordon SR. Occlusion rate and complications of plastic biliary stent placement in patients undergoing neoadjuvant chemoradiotherapy or pancreatic cancer with malignant biliary obstruction. J Clin Gastroenterol 2010;44:452-5. [PubMed]
- Tierney J, Bhutiani N, Stamp B, et al. Predictive risk factors associated with cholangitis following ERCP. Surg Endosc 2018;32:799-804. [Crossref] [PubMed]
- Iyer R. Cholangocarcinoma Foundation. Biliary Emergency Information Card {Internet}. US; 2013. Available online: https://cholangiocarcinoma.org/biliary-emergency-information-card/


