Intrahepatic cholangiocarcinoma: the AJCC/UICC 8th edition updates
Intrahepatic cholangiocarcinoma is the second most common primary liver cancer after hepatocellular carcinoma and is increasing in incidence worldwide (1). Surgical resection is the only potentially curative therapy and results in 5-year overall survival rates between 15% and 40% (2). Unfortunately, disease relapse after resection occurs in up to two-thirds of patients (3). Prognostic factors associated with higher recurrence include positive surgical margin, lymph node metastasis, vascular invasion, and multiple tumors (4,5). The American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) staging system represents a standard for stratifying patients with cancer, predicting prognosis, and guiding treatment decisions (6). The recently published 8th edition of the AJCC Staging Manual represents the first revision of the previously novel staging of intrahepatic cholangiocarcinoma introduced in the 7th edition (7). Before the 7th edition, intrahepatic cholangiocarcinoma shared the same staging as hepatocellular carcinoma.
Both the 7th and 8th editions of the AJCC Staging Manual recommend data collection of tumor growth patterns, classified as mass-forming, periductal-infiltrating, or mixed types, based on the Liver Cancer Study Group of Japan (LCSGJ) classification (8). The LCSGJ also defines an intraductal growth type, which is rare and associated with a favorable prognosis. The mass-forming type is the most common and characterized by an intraparenchymal mass with distinct borders. The periductal-infiltrating type is marked by tumor infiltration along the bile duct, often causing dilatation of a peripheral bile duct. Some studies show worse survival after resection of the periductal-infiltrating type compared with the mass-forming type, whereas other reports show no difference in survival (5,9-11). Recently, histologic studies have divided intrahepatic cholangiocarcinoma into large duct and small duct subtypes, which correlate with macroscopic growth patterns (12,13). The small duct type is found in mass-forming tumors and is associated with chronic liver disease. The large duct type occurs in patients with chronic biliary disease and exhibits a variable macroscopic growth pattern.
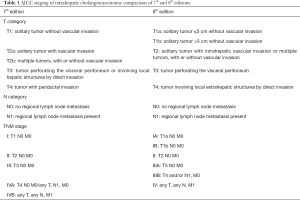
AJCC 7th edition
The 7th edition of the AJCC staging system for intrahepatic cholangiocarcinoma included tumor number, vascular invasion, and direct extrahepatic extension as defining components of the T category (Table 1) (7). Tumors with periductal invasion were classified as T4, stage IVA. This T4 classification was based on limited analyses suggesting a prognostic significance of tumor growth patterns for intrahepatic cholangiocarcinoma (9). Compared to the more common mass-forming type, periductal-infiltrating type of intrahepatic cholangiocarcinoma is reportedly associated with a poor prognosis. The T4 category included diffuse periductal-infiltrating tumors and mixed mass-forming plus periductal-infiltrating tumors. The 7th edition of the AJCC staging system was validated in several independent patient populations (14,15).
Full table
Changes in AJCC 8th edition
Significant changes in the 8th edition of the AJCC staging of intrahepatic cholangiocarcinoma are presented below.
Size
The revised AJCC 8th edition incorporated a tumor size cutoff of 5 cm to separate the T1 category into T1a and T1b subgroups. Institutional and registry studies have shown that maximum tumor diameter >5 cm is an independent prognostic factor for overall survival (5,16,17). Furthermore, tumor size >5 cm is associated with microscopic vascular invasion and higher tumor grade (18).
Serosal invasion
In both the 7th and 8th editions of the AJCC staging system of intrahepatic cholangiocarcinoma, the T3 category is defined as perforation of the visceral peritoneum. The LCSGJ staging system also includes serosal invasion as a component of the T category (8).
T4 category
In the 7th edition, periductal invasion defined the T4 category and was classified as stage IVA. For the 8th edition, periductal invasion is removed from the T4 category because of a lack of recent data on the prognostic effect of periductal invasion. T4 is now defined as tumor involving local extrahepatic structures by direct invasion and is categorized as stage IIIB. Sakamoto et al. reported that in patients undergoing resection of intrahepatic cholangiocarcinoma, invasion of the first-order branch of the bile duct is an independent factor for worse prognosis (19). However, other surgical series on intrahepatic cholangiocarcinoma exclude tumors involving the hepatic hilum from analysis (8,20).
The definition of periductal invasion remains an area of controversy. The 7th and 8th editions of the AJCC Staging Manual define intrahepatic cholangiocarcinoma anatomically as extending from the periphery of the liver to the second-order bile ducts. This definition does not differentiate between hilar cholangiocarcinoma with an intrahepatic component and intrahepatic cholangiocarcinoma involving the hepatic hilum. A solution to this ambiguous definition proposed by Ebata et al. is to define the center of the tumor in relation to the umbilical portion of the left portal vein and the right posterior portal vein as anatomic boundaries for the hilar bile duct (21).
Tumor number and vascular invasion
The 7th edition T2 category was subdivided into T2a, solitary tumor with vascular invasion, and T2b, multiple tumors, with or without vascular invasion. In the 8th edition, the T2 category is no longer subdivided, indicating an equivalent prognostic effect of vascular invasion and multifocal disease.
Lymph nodes
In the 7th edition, intrahepatic cholangiocarcinoma with regional lymph node metastasis was classified as stage IVA. In surgical series, up to one-third of patients have node-positive disease (22). For the 8th edition, regional lymph node metastasis was downstaged from IVA to IIIB. A challenge with the N1 category in intrahepatic cholangiocarcinoma is that routine lymphadenectomy is not standardized across institutions. According to an analysis of the Surveillance, Epidemiology, and End Results (SEER) database, information on lymph node status was available in only 49% of patients undergoing resection of intrahepatic cholangiocarcinoma (23). In addition, there are no guidelines on the minimum number of lymph nodes that should be harvested. In the 8th edition of the AJCC staging of intrahepatic cholangiocarcinoma, recovery of at least 6 lymph nodes is recommended for complete nodal staging, consistent with recommendations for gallbladder cancer.
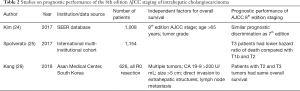
Validation of AJCC 8th edition staging of intrahepatic cholangiocarcinoma
Three studies have been published on the prognostic value of the 8th edition of the AJCC staging for intrahepatic cholangiocarcinoma (Table 2) (24-26). These studies show that the new 8th edition is similar or better than the 7th edition in stratifying patients’ overall survival.
Full table
An analysis by Kim et al. of the SEER registry found that the 8th edition was comparable to the 7th edition (24). Harrell’s concordance index for overall survival was 0.669 for the 8th edition and 0.667 for the 7th edition.
Spolverato et al. evaluated the 8th edition of the AJCC staging using a multi-institutional cohort of patients who underwent curative-intent hepatic resection (25). Compared to the 7th edition, the 8th edition staging was able to better stratify survival in stage III patients. Paradoxically, patients categorized by the 8th edition staging with T3 tumors had 5-year overall survival rates that surpassed those of patients with T1b and T2 tumors. The T3 category is defined as perforation of the visceral peritoneum, or serosal invasion. The LCSGJ staging system also includes serosal invasion as a component of the T category (8). Sakamoto et al. proposed removing serosal invasion from the LCSGJ staging system, since serosal invasion was not significantly associated with survival (19).
Kang et al. assessed the prognostic impact of the 8th edition AJCC staging of intrahepatic cholangiocarcinoma and found that in patients without lymph node metastasis, median overall survival rates with T2 and T3 tumors were 25 months and 27 months, respectively (26). Median time to recurrence with T2 and T3 tumors was 14 and 15 months, respectively. Similar to the findings by Spolverato et al., this study suggests that the 8th edition T3 category does not accurately reflect patient prognosis and tumor biology.
Conclusions
The revisions to staging of intrahepatic cholangiocarcinoma in the 8th edition of the AJCC Staging Manual build upon the foundation of the 7th edition, which represented the first unique AJCC staging for intrahepatic cholangiocarcinoma. These revisions were based upon detailed pathologic analysis of resected surgical specimens from international hepatobiliary centers of excellence. The future 9th edition will be further improved by continued international efforts to share and rigorously analyze data.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shaib YH, Davila JA, McGlynn K, et al. Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? J Hepatol 2004;40:472-7. [Crossref] [PubMed]
- Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol 2014;60:1268-89. [Crossref] [PubMed]
- Spolverato G, Vitale A, Cucchetti A, et al. Can hepatic resection provide a long-term cure for patients with intrahepatic cholangiocarcinoma? Cancer 2015;121:3998-4006. [Crossref] [PubMed]
- Wang Y, Li J, Xia Y, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol 2013;31:1188-95. [Crossref] [PubMed]
- Hwang S, Lee YJ, Song GW, et al. Prognostic Impact of Tumor Growth Type on 7th AJCC Staging System for Intrahepatic Cholangiocarcinoma: a Single-Center Experience of 659 Cases. J Gastrointest Surg 2015;19:1291-304. [Crossref] [PubMed]
- Amin MB. American Joint Committee on Cancer, American Cancer Society. AJCC cancer staging manual. Eight edition. Chicago, IL American Joint Committee on Cancer, Springer 2017;xvii:1024.
- Edge SB, American Joint Committee on Cancer. AJCC cancer staging manual. 7th ed. New York: Springer, 2010:xiv, 648.
- Yamasaki S. Intrahepatic cholangiocarcinoma: macroscopic type and stage classification. J Hepatobiliary Pancreat Surg 2003;10:288-91. [Crossref] [PubMed]
- Shimada K, Sano T, Sakamoto Y, et al. Surgical outcomes of the mass-forming plus periductal infiltrating types of intrahepatic cholangiocarcinoma: a comparative study with the typical mass-forming type of intrahepatic cholangiocarcinoma. World J Surg 2007;31:2016-22. [Crossref] [PubMed]
- Yamamoto M, Takasaki K, Yoshikawa T, et al. Does gross appearance indicate prognosis in intrahepatic cholangiocarcinoma? J Surg Oncol 1998;69:162-7. [Crossref] [PubMed]
- Ohtsuka M, Ito H, Kimura F, et al. Results of surgical treatment for intrahepatic cholangiocarcinoma and clinicopathological factors influencing survival. Br J Surg 2002;89:1525-31. [Crossref] [PubMed]
- Hayashi A, Misumi K, Shibahara J, et al. Distinct Clinicopathologic and Genetic Features of 2 Histologic Subtypes of Intrahepatic Cholangiocarcinoma. Am J Surg Pathol 2016;40:1021-30. [Crossref] [PubMed]
- Aishima S, Oda Y. Pathogenesis and classification of intrahepatic cholangiocarcinoma: different characters of perihilar large duct type versus peripheral small duct type. J Hepatobiliary Pancreat Sci 2015;22:94-100. [Crossref] [PubMed]
- Farges O, Fuks D, Le Treut YP, et al. AJCC 7th edition of TNM staging accurately discriminates outcomes of patients with resectable intrahepatic cholangiocarcinoma: By the AFC-IHCC-2009 study group. Cancer 2011;117:2170-7.
- Ribero D, Nuzzo G, Amisano M, et al. Comparison of the prognostic accuracy of the sixth and seventh editions of the TNM classification for intrahepatic cholangiocarcinoma. HPB (Oxford) 2011;13:198-205.
- Ali SM, Clark CJ, Mounajjed T, et al. Model to predict survival after surgical resection of intrahepatic cholangiocarcinoma: the Mayo Clinic experience. HPB (Oxford) 2015;17:244-50. [Crossref] [PubMed]
- Doussot A, Gonen M, Wiggers JK, et al. Recurrence Patterns and Disease-Free Survival after Resection of Intrahepatic Cholangiocarcinoma: Preoperative and Postoperative Prognostic Models. J Am Coll Surg 2016;223:493-505.e2. [Crossref] [PubMed]
- Spolverato G, Ejaz A, Kim Y, et al. Tumor size predicts vascular invasion and histologic grade among patients undergoing resection of intrahepatic cholangiocarcinoma. J Gastrointest Surg 2014;18:1284-91. [Crossref] [PubMed]
- Sakamoto Y, Kokudo N, Matsuyama Y, et al. Proposal of a new staging system for intrahepatic cholangiocarcinoma: Analysis of surgical patients from a nationwide survey of the Liver Cancer Study Group of Japan. Cancer 2016;122:61-70. [Crossref] [PubMed]
- Igami T, Ebata T, Yokoyama Y, et al. Staging of peripheral-type intrahepatic cholangiocarcinoma: appraisal of the new TNM classification and its modifications. World J Surg 2011;35:2501-9. [Crossref] [PubMed]
- Ebata T, Kosuge T, Hirano S, et al. Proposal to modify the International Union Against Cancer staging system for perihilar cholangiocarcinomas. Br J Surg 2014;101:79-88. [Crossref] [PubMed]
- de Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol 2011;29:3140-5. [Crossref] [PubMed]
- Clark CJ, Wood-Wentz CM, Reid-Lombardo KM, et al. Lymphadenectomy in the staging and treatment of intrahepatic cholangiocarcinoma: a population-based study using the National Cancer Institute SEER database. HPB (Oxford) 2011;13:612-20. [Crossref] [PubMed]
- Kim Y, Moris DP, Zhang XF, et al. Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: A surveillance, epidemiology, and end results (SEER) analysis. J Surg Oncol 2017;116:643-50.
- Spolverato G, Bagante F, Weiss M, et al. Comparative performances of the 7th and the 8th editions of the American Joint Committee on Cancer staging systems for intrahepatic cholangiocarcinoma. J Surg Oncol 2017;115:696-703.
- Kang SH, Hwang S, Lee YJ, et al. Prognostic comparison of the 7th and 8th editions of the American Joint Committee on Cancer staging system for intrahepatic cholangiocarcinoma. J Hepatobiliary Pancreat Sci 2018;25:240-8.


