A novel diagnostic biomarker for human uterine leiomyosarcoma: PSMB9/β1i
Takuma Hayashi (Shinshu University School of Medicine) discussed a novel biomarker for detecting human uterine leiomyosarcoma (LMS). Patients with uterine LMS typically present with vaginal bleeding, pain and a pelvic mass, with atypical presentations of hypercalcemia and eosinophilia also being reported (1-3). There is concern that radiographic evaluation with combined positron emission tomography/computed tomography, which is commonly used to aid assessment of patient prognosis, might not necessarily be effective for diagnosis and surveillance of human uterine LMS (4-6). Unfortunately, radiographic imaging cannot provide any medical information to help distinguish between benign leiomyoma (LMA) and malignant human uterine LMS (7).
Importantly, diagnostic biomarkers that are able to distinguish between human uterine LMS and LMA are not yet established. The mice with a targeted disruption of proteasome subunit beta type (PSMB) 9/β1i, which is IFN-γ-inducible proteasome beta subunit, exhibited a defect in tissue- and substrate-dependent proteasome function, Hayashi’s research group reports that PSMB9/β1i-deficient mice exhibit spontaneous development of human uterine LMS, with a disease prevalence of ~37% by 12 months of age (8,9). The current focus of Hayashi’s research is to probe the loss of PSMB9/β1i expression in human uterine LMS, as well as the detectable expression of the protein in human LMA (10,11). Defective expression of PSMB9/β1i is likely to be one of the risk factors for the development of human uterine neoplasms, as it is in the PSMB9-deficient mouse. Thus, PSMB9/β1i is useful as a novel diagnostic biomarker for human uterine LMS, and Hayashi’s research group have been trying to establish a novel diagnostic biomarker with PSMB9/β1i, which can distinguish the human uterine LMS from other human uterine mesenchymal tumours including LMA under the SIGMA-Aldrich Collaboration Laboratory Project.
The immunohistochemistry (IHC) experiments, performed separately at several medical facilities, revealed a serious loss in the ability to induce PSMB9/β1i expression in human uterine LMS tissues in comparison with normal human myometrium tissues located in same tissue sections: normal myometrium; total 73 cases, uterine LMA; total 52 cases, Bizarre LMA; total 3 cases, uterine LMS; total 58 cases. Of the 58 patients with uterine LMS that we examined, 49 were negative for PSMB9/β1i expression, 4 were focally positive, and 3 were partially positive. Two patients with uterine LMS were analyzed for PSMB9/β1i expression (10,11) (Table 1). PSMB9/β1i levels were also evaluated in skeletal muscle and rectal metastases from individual patients with uterine LMS, where surgical samples showed the presence of a mass measuring 3 cm in maximum diameter in the lumbar quadrate muscle without a fibrous capsule. All lymph nodes were negative for LMS metastases, and IHC analyses showed positivity for Ki-67 (clone MIB1) and negativity for PSMB9/β1i. The defective PSMB9/β1i expression detected in primary uterine LMS was also observed in the metastatic LMS of the skeletal muscle and rectum, indicating that the metastatic lesions conserved this biological characteristic of primary uterine LMS. In both western blotting and RT-PCR experiments, PSMB9/β1i was expressed in uterine LMA, Bizarre LMA and normal myometrium but not in human uterine LMS, which was strongly supportive of the IHC findings. Furthermore, analysis of a human uterine LMS cell line clarified the biological significance of PSMB9/β1i in malignant myometrium transformation and cell cycle, thus implicating PSMB9/β1i as an anti-tumorigenic candidate (10,11). Uterine LMS reportedly is a highly metastatic smooth muscle neoplasm for which calponin h1 is suspected to have a biological role as a tumor-suppressor. Moreover, several lines of evidence indicate that although calponin h1 does not directly influence tumorigenesis, it clearly affects PSMB9/β1i-induced cellular morphological changes (12). This role of PSMB9/β1i as a tumor suppressor may lead to new therapeutic targets in human uterine LMS.
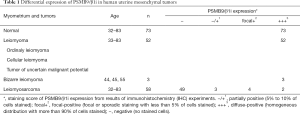
Full table
Conclusions
Defective PSMB9/β1i expression is likely to be one of the risk factors for the development of human uterine neoplasm, as it is in the PSMB9/β1i deficient mouse. Thus, combination of PSMB9/β1i with other functional candidates is useful for a novel diagnostic biomarker for human uterine LMS (13-15). Additionally, gene therapy with PSMB9/β1i expression vectors may be a new treatment for human uterine LMS that exhibit a defect in PSMB9/β1i expression. Because there is no effective therapy for unresectable uterine LMS, our results may bring us to specific molecular therapies to treat this disease.
Experimental procedure
IHC was performed using the avidin-biotin complex method previously described. Briefly, one representative 5-µm tissue section was cut from a paraffin-embedded sample of the radical hysterectomy specimen from 58 patients with uterine LMS, 52 patients with LMA, 3 patients with Bizarre LMA, normal myometrium total 73 cases. Sections were deparaffinized and rehydrated in graded alcohols and then incubated with normal mouse serum for 20 min. Sections were incubated at room temperature for 1 h with anti-human PSMB9/β1i antibody (SIGMA-Aldrich Israel, Rehovot, Israel, dilution 1/100). Afterwards, sections were incubated with a biotinylated secondary antibody (Dako, Carpinteria, CA, USA) and then exposed to a streptavidin complex (Dako). Complete reaction was revealed by 3,3’-diaminobenzidine, and the slide was counterstained with hematoxylin. Twenty one normal human myometrium sections from specimens were used as positive controls. Negative controls consisted of tissue sections also incubated with normal rabbit IgG instead of the primary antibody.
Acknowledgements
We sincerely appreciate the generous donation of PSMB9/β1i-deficient breeding mice and technical comments by Dr. Luc Van Kaer and Dr. Susumu Tonegawa, Massachusetts Institute of Technology. We thank Isamu Ishiwata for his generous gift of the human Ut-LMS cell lines. We appreciate the technical assistance of the research staff at Harvard Medical School. We are grateful to Dr. Tamotsu Sudo and Dr. Ryuichiro Nishimura, Hyogo Cancer Center for Adults for their generous assistance with immunohistochemistry (IHC) analysis and helpful discussion.
Funding: This work was supported by grants from the Ministry of Education, Culture, Science and Technology (No. 15K10709), the Japan Science and Technology Agency, the Foundation for the Promotion of Cancer Research, Kanzawa Medical Research Foundation, and The Ichiro Kanehara Foundation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Zaloudek C, Hendrickson MR. In: Kurman RJ. editor. Mesenchymal tumors of the uterus: Blaustein’s Pathology of the Female Genital Tract. ed 5. New York: Springer-Verlag, 2002:561-78.
- Gadducci A, Landoni F, Sartori E, et al. Uterine leiomyosarcoma: analysis of treatment failures and survival. Gynecol Oncol 1996;62:25-32. [Crossref] [PubMed]
- Nordal RR, Thoresen SO. Uterine sarcomas in Norway 1956-1992: incidence, survival and mortality. Eur J Cancer 1997;33:907-11. [Crossref] [PubMed]
- Wu TI, Chang TC, Hsueh S, et al. Prognostic factors and impact of adjuvant chemotherapy for uterine leiomyosarcoma. Gynecol Oncol 2006;100:166-72. [Crossref] [PubMed]
- Leitao MM, Soslow RA, Nonaka D, et al. Tissue microarray immunohistochemical expression of estrogen, progesterone, and androgen receptors in uterine leiomyomata and leiomyosarcoma. Cancer 2004;101:1455-62. [Crossref] [PubMed]
- Kurma RJ. Blaustein's Pathology of the Female Genital Tract, 4th ed. New York: Springer-Verlag, 2001:499.
- Diagnostic Criteria for LMS, Adapted from 2003 WHO Guidelines: World Health Organization Classification of Tumours: Pathology and Genetics, Pathology and Genetics of Tumours of the Breast and Female Genital Organs. France: IARC Press, 2003.
- Van Kaer L, Ashton-Rickardt PG, Eichelberger M, et al. Altered peptidase and viral-specific T cell response in LMP2 mutant mice. Immunity 1994;1:533-41. [Crossref] [PubMed]
- Hayashi T, Faustman DL. Development of spontaneous uterine tumors in low molecular mass polypeptide-2 knockout mice. Cancer Res 2002;62:24-7. [PubMed]
- Hayashi T, Kobayashi Y, Kohsaka S, et al. The mutation in the ATP-binding region of JAK1, identified in human uterine leiomyosarcomas, results in defective interferon-gamma inducibility of TAP1 and LMP2. Oncogene 2006;25:4016-26. [Crossref] [PubMed]
- Hayashi T, Horiuchi A, Sano K, et al. Potential role of LMP2 as tumor-suppressor defines new targets for uterine leiomyosarcoma therapy. Sci Rep 2011;1:180. [Crossref] [PubMed]
- Hayashi T, Horiuchi A, Sano K, et al. Potential role of LMP2 as an anti-oncogenic factor in human uterine leiomyosarcoma: morphological significance of calponin h1. FEBS Lett 2012;586:1824-31. [Crossref] [PubMed]
- Hayashi T, Ichimura T, Yaegashi N, et al. Expression of CAVEOLIN 1 in uterine mesenchymal tumors: No relationship between malignancy and CAVEOLIN 1 expression. Biochem Biophys Res Commun 2015;463:982-7. [Crossref] [PubMed]
- Hayashi T, Horiuchi A, Sano K, et al. Potential diagnostic biomarkers: differential expression of LMP2/β1i and cyclin B1 in human uterine leiomyosarcoma. Tumori 2014;100:99e-106e. [PubMed]
- Kawano M, Hayashi T. Bioological Analysis for Understanding of the Uterine Sarcomagenesis. Global Journal for Research Analysis 2016;5:310-1.


